Reproductive Hormonal Disorders
This group of endocrine diseases includes the following conditions
- Polycystic Ovary Syndrome (PCOS)
- Hypogonadism (Male and Female)
- Premature Ovarian Insufficiency (POI)
- Hyperprolactinemia (also described under pituitary diseases)
- Erectile Dysfunction (hormonal causes)
- Infertility (hormonal causes)
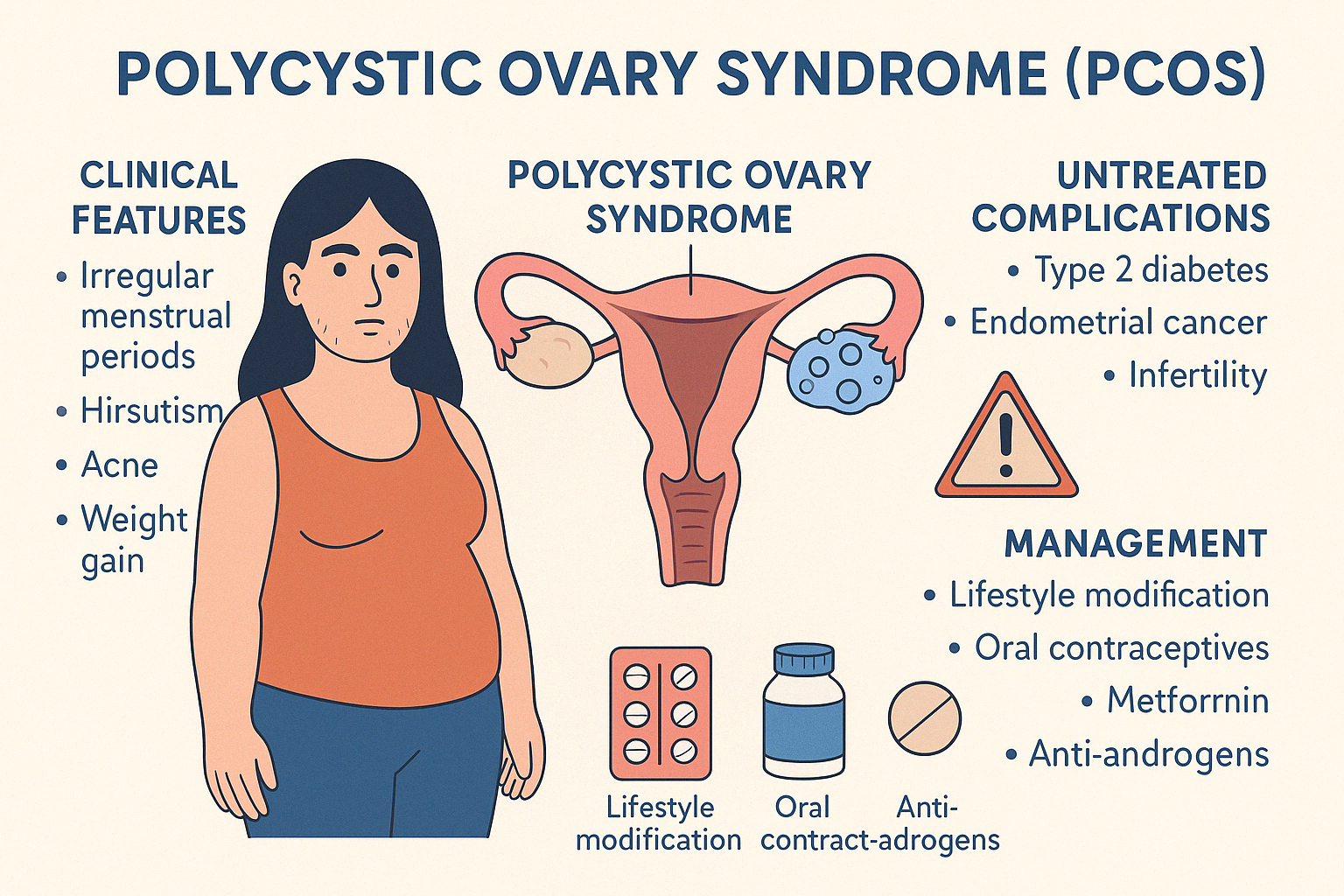
1. Polycystic Ovary Syndrome (PCOS)
Polycystic Ovary Syndrome (PCOS) is one of the most common endocrine disorders in women of reproductive age. It is characterized by chronic anovulation, excess androgen levels, and polycystic ovaries, though not all three features are required for diagnosis.
The exact cause of PCOS remains unclear, but it is believed to involve a combination of genetic predisposition, insulin resistance, and hormonal imbalances. Insulin resistance plays a central role in many patients, contributing to increased androgen production by the ovaries.
Clinical Features
Common symptoms include:
- Irregular or absent menstrual periods
- Hirsutism (excess facial and body hair)
- Acne and oily skin
- Weight gain, especially central obesity
- Hair thinning or male-pattern baldness
- Infertility
Ultrasound may reveal multiple small follicles (polycystic ovaries), though this is not always present.
Complications if Untreated
- Type 2 Diabetes and metabolic syndrome
- Endometrial hyperplasia and cancer (due to unopposed estrogen)
- Dyslipidemia and cardiovascular risk
- Infertility and pregnancy complications
Diagnosis
Based on the Rotterdam Criteria, diagnosis requires any two out of three:
- Oligo- or anovulation
- Clinical/biochemical signs of hyperandrogenism
- Polycystic ovaries on ultrasound
Management
Treatment is individualized and includes:
- Lifestyle modification (diet and exercise)
- Oral contraceptives for menstrual regularity and hyperandrogenism
- Metformin for insulin resistance
- Anti-androgens (e.g., spironolactone) for hirsutism
- Ovulation induction agents (e.g., letrozole or clomiphene) for fertility
PCOS is a chronic condition, but with a multidisciplinary approach, its symptoms and risks can be effectively managed.
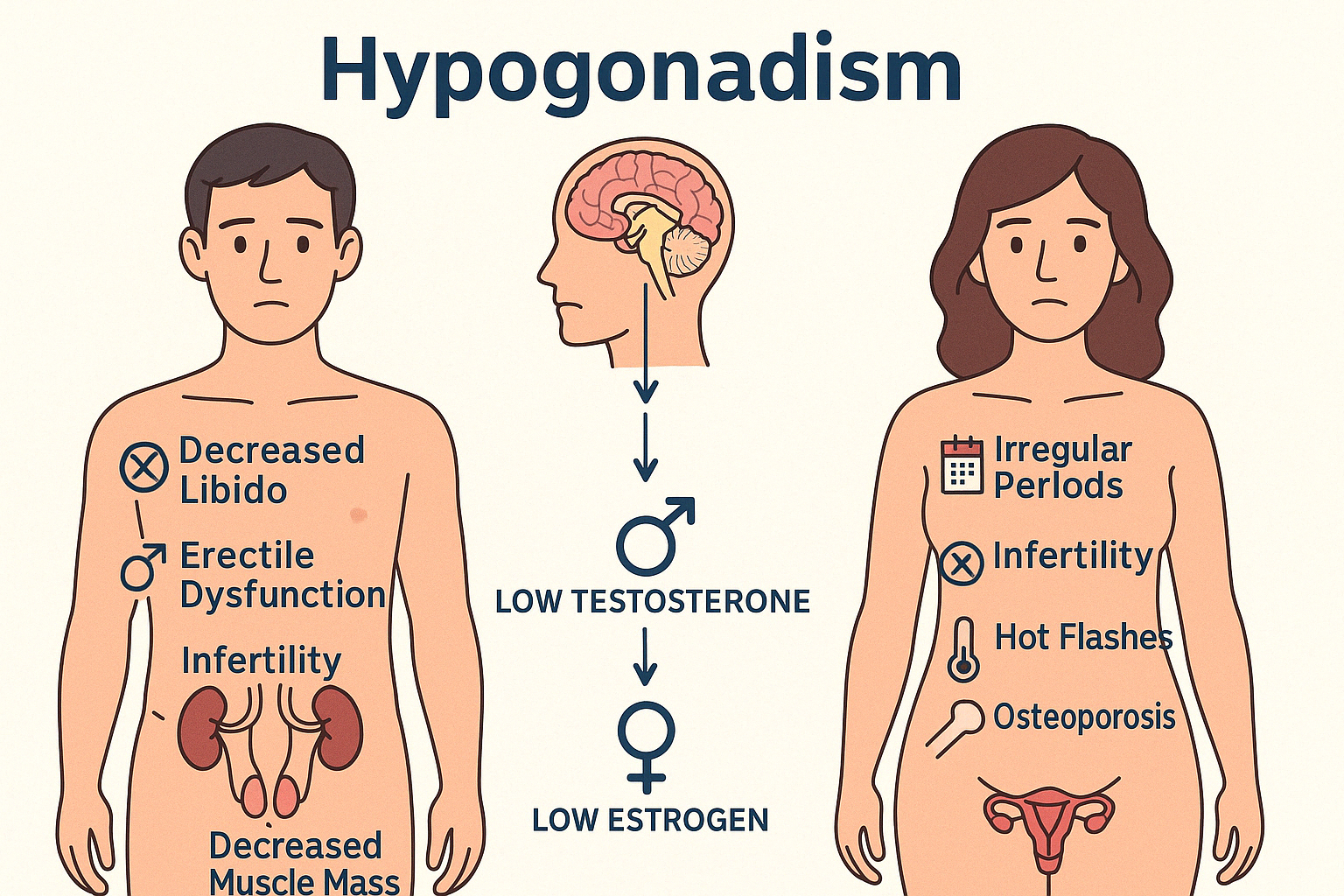
2. Hypogonadism (Male and Female)
Hypogonadism refers to reduced or absent secretion of sex hormones — testosterone in males and estrogen/progesterone in females — due to dysfunction of the gonads or the hypothalamic-pituitary axis.
It is classified into:
- Primary (Hypergonadotropic): Problem in the gonads themselves
- Secondary (Hypogonadotropic): Problem in the hypothalamus or pituitary
Causes
- Genetic disorders (Klinefelter, Turner, Kallmann syndrome)
- Pituitary tumors or trauma
- Chemotherapy, radiation, infections
- Chronic illnesses or malnutrition
Clinical Features
In males:
- Delayed puberty or absent secondary sexual characteristics
- Decreased libido and erectile dysfunction
- Infertility
- Decreased muscle mass and body hair
- Osteoporosis or gynecomastia
In females:
- Delayed puberty, primary amenorrhea
- Irregular or absent periods
- Infertility
- Hot flashes and vaginal dryness
- Low bone density
Diagnosis
- Low serum testosterone in males or estradiol in females
- FSH and LH help distinguish primary from secondary hypogonadism
- Imaging (MRI of pituitary) in selected cases
Treatment
- Hormone replacement therapy (testosterone in men, estrogen ± progesterone in women)
- Fertility options (hCG, gonadotropins, pulsatile GnRH) if desired
- Addressing underlying cause (e.g., pituitary tumor, lifestyle factors)
With proper diagnosis and individualized management, hypogonadism can be effectively treated, improving both quality of life and reproductive outcomes.
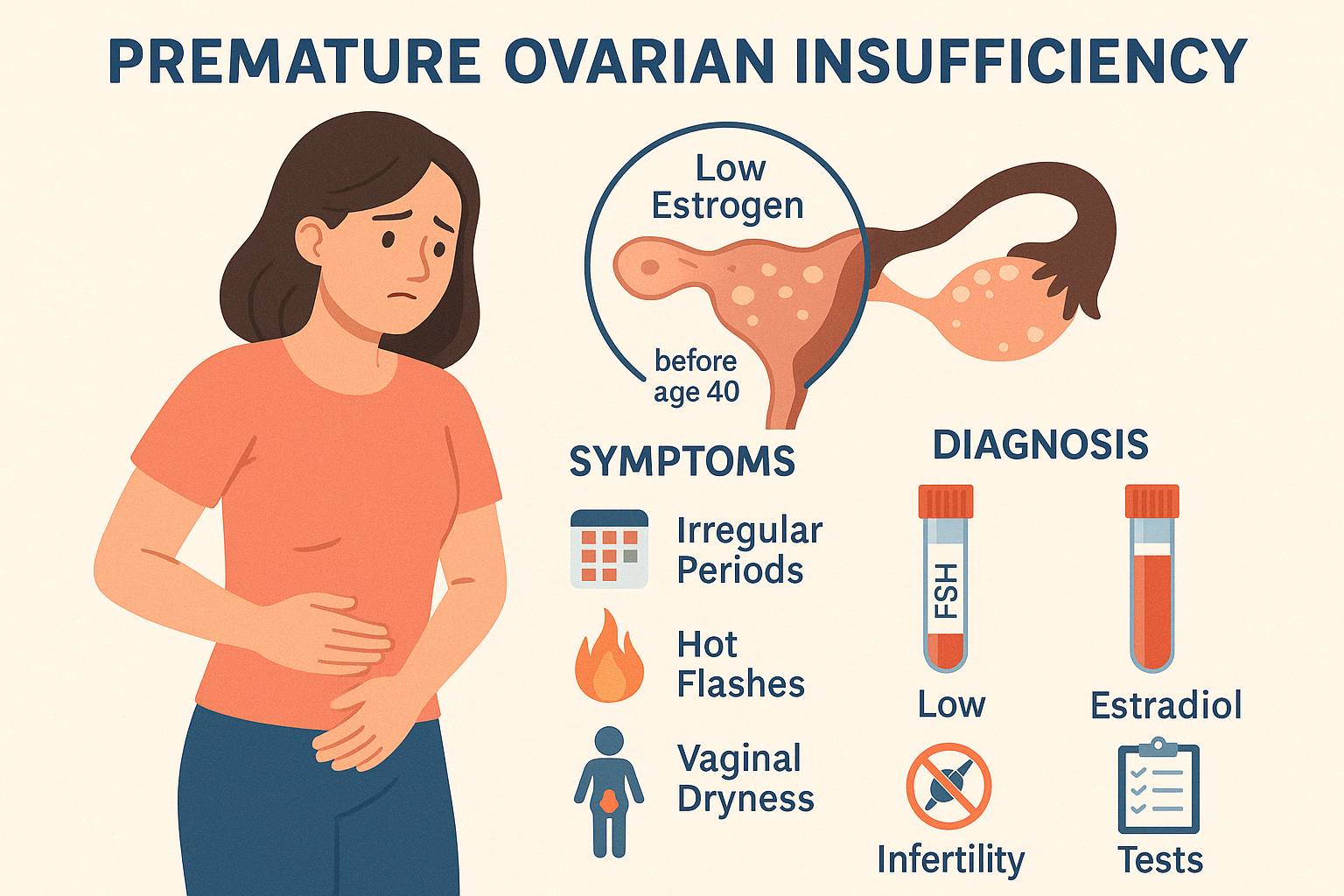
3. Premature Ovarian Insufficiency (POI)
Premature Ovarian Insufficiency (POI), also known as premature ovarian failure, refers to the loss of normal ovarian function before the age of 40. It results in low estrogen levels, irregular or absent menstrual periods, and often, infertility.
While the exact cause is unknown in many cases, contributing factors include:
- Genetic conditions (e.g., Turner syndrome, fragile X premutation)
- Autoimmune diseases
- Chemotherapy or radiation therapy
- Infections (rarely, such as mumps oophoritis)
- Idiopathic (no identifiable cause)
Clinical Presentation
- Irregular or missed periods (oligomenorrhea or amenorrhea)
- Hot flashes and night sweats
- Vaginal dryness, pain during intercourse
- Infertility
- Mood changes and fatigue
- Decreased bone density (osteopenia/osteoporosis)
Diagnosis
- Elevated FSH levels (in menopausal range) on two separate occasions
- Low estradiol levels
- History and exam to rule out other causes of amenorrhea
- Genetic and autoimmune testing as indicated
Complications
- Infertility
- Early onset osteoporosis
- Cardiovascular risk
- Emotional and psychological impact
Management
- Hormone replacement therapy (HRT) to relieve symptoms and protect bone and heart health
- Calcium and vitamin D supplementation
- Fertility counseling: spontaneous pregnancy can occur in 5–10% of cases; assisted reproductive technologies or donor eggs are options
- Emotional support and counseling
With timely diagnosis and personalized care, women with POI can lead healthy, fulfilling lives.
Engage With Dr. Vipin Mishra
Whether you are dealing with chronic endocrine condition or just want to understand your body better, or wish to obtain an exalted consciousness, you can take help and guidance from Dr. Vipin Mishra.
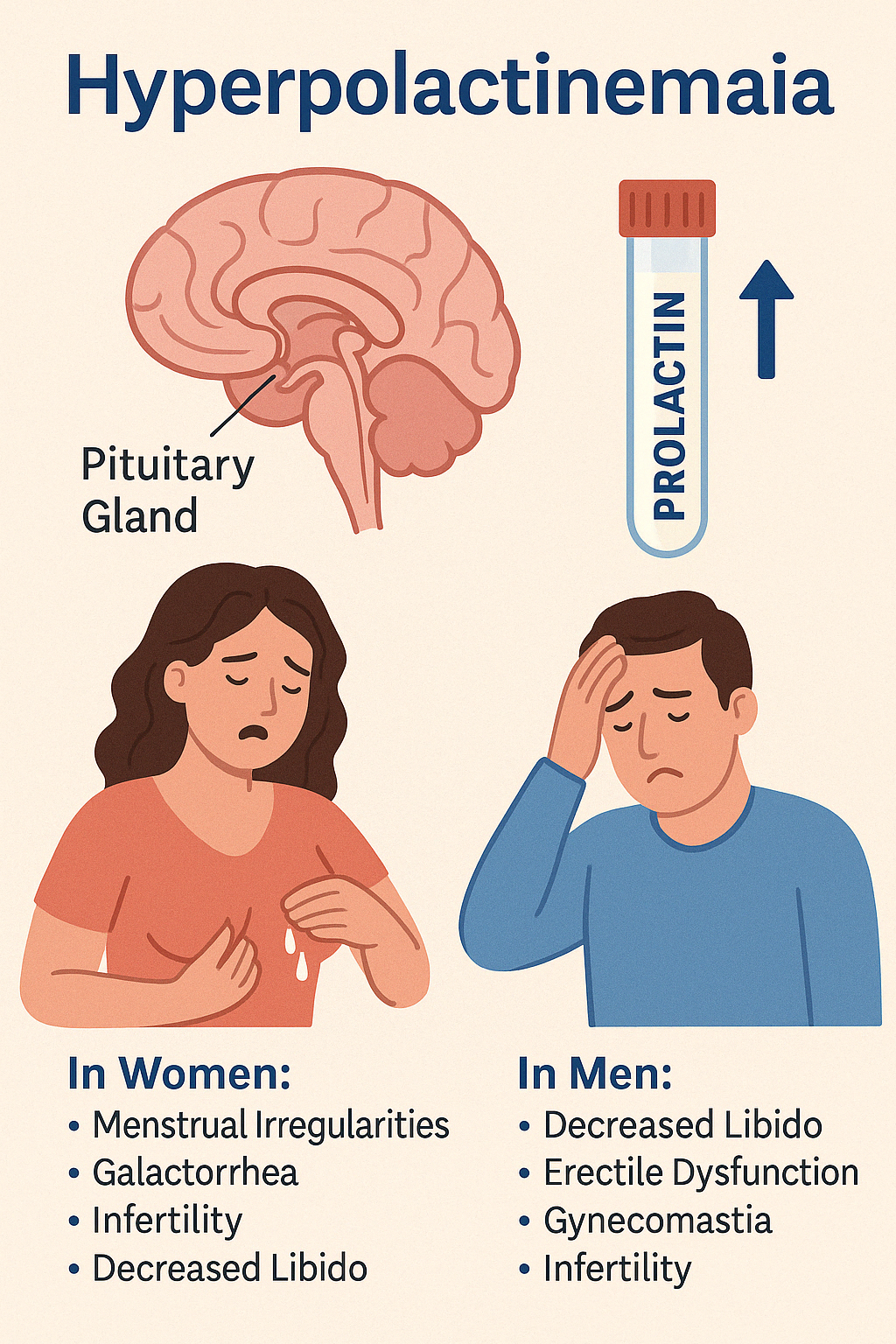
Engage With Dr. Vipin Mishra4. Hyperprolactinemia
Hyperprolactinemia is a condition characterized by elevated levels of prolactin, a hormone secreted by the anterior pituitary gland. Prolactin plays a primary role in lactation, but its excess can disrupt the reproductive axis and affect both men and women.
Causes
- Prolactin-secreting pituitary tumors (prolactinomas)
- Hypothyroidism
- Chronic renal failure
- Chest wall trauma or surgery
- Medications (e.g., antipsychotics, antidepressants, antiemetics)
- Stress or macroprolactinemia (biologically inactive forms)
Clinical Features
In women:
- Menstrual irregularities (oligomenorrhea or amenorrhea)
- Galactorrhea (milk discharge from the breast not related to childbirth)
- Infertility
- Decreased libido
In men:
- Decreased libido
- Erectile dysfunction
- Gynecomastia
- Infertility
- Sometimes galactorrhea (rare)
In both sexes, large prolactinomas may cause headaches and visual disturbances (bitemporal hemianopia) due to optic chiasm compression.
Diagnosis
- Elevated serum prolactin levels (repeat testing if needed)
- Pituitary MRI to assess for prolactinoma
- Rule out hypothyroidism and other causes
Management
- Dopamine agonists (e.g., cabergoline, bromocriptine) are first-line therapy and often shrink tumors
- Surgical resection for drug-resistant or symptomatic macroadenomas
- Treat underlying causes (e.g., correcting hypothyroidism or adjusting medications)
Hyperprolactinemia is highly treatable, and timely intervention restores normal reproductive function in most patients.
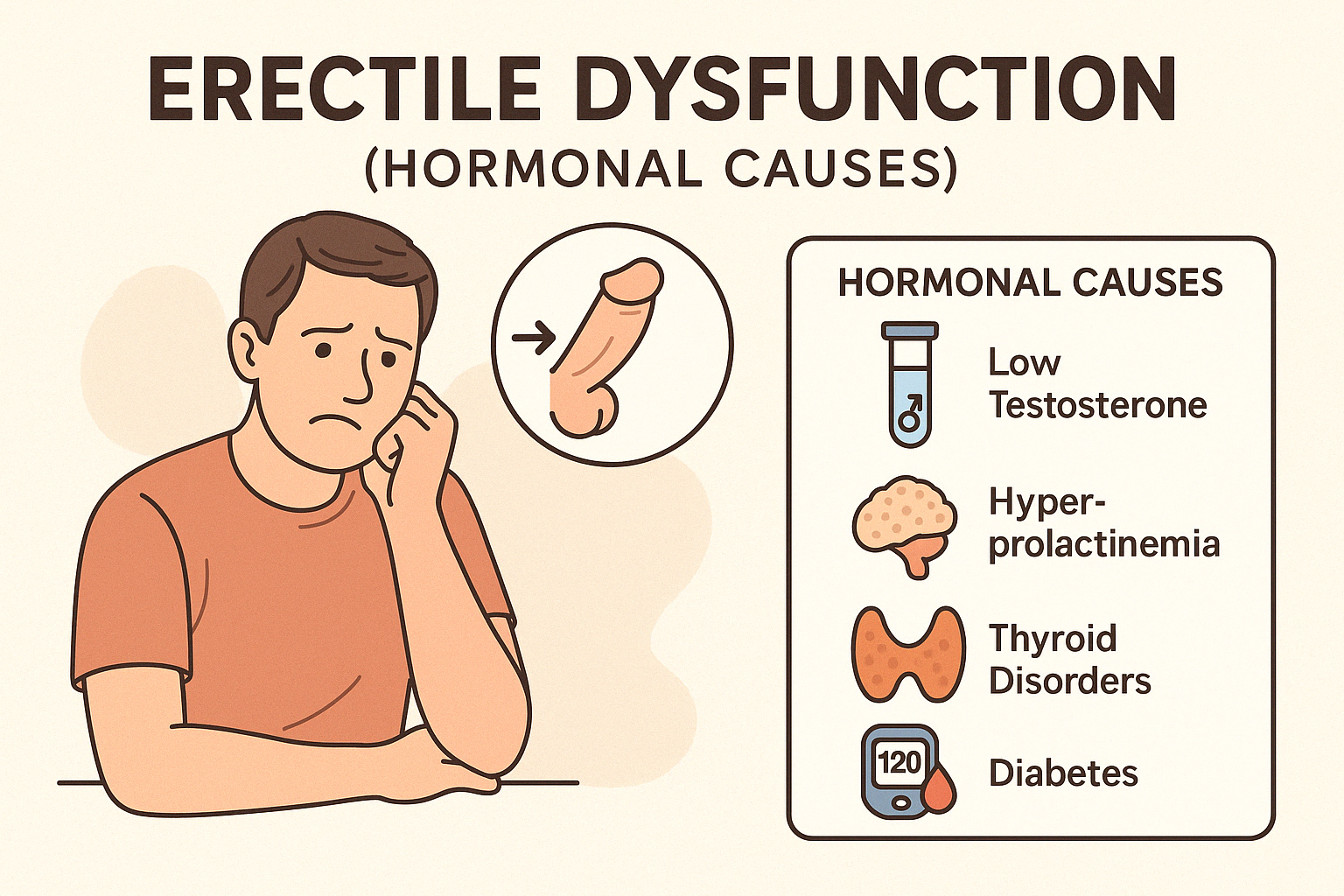
5. Erectile Dysfunction (hormonal causes)
Erectile Dysfunction (ED) is the persistent inability to attain or maintain an erection sufficient for satisfactory sexual performance. While vascular and psychological factors are common, hormonal imbalances can also play a key role and are often overlooked.
Hormonal Causes of ED
- Low testosterone (hypogonadism) — reduces libido and impairs erection quality
- Hyperprolactinemia — suppresses gonadotropin release, lowering testosterone
- Thyroid disorders — both hyperthyroidism and hypothyroidism can affect erectile function
- Cushing's syndrome and diabetes — impact the hypothalamic-pituitary-gonadal axis
Clinical Features
- Reduced libido
- Difficulty achieving or maintaining erections
- Fatigue or decreased stamina
- Depressed mood or lack of motivation
- Other signs of underlying endocrine disorder (e.g., gynecomastia, testicular atrophy, weight changes)
Diagnosis
- Serum testosterone levels (morning sample)
- LH and FSH to differentiate primary vs. secondary hypogonadism
- Prolactin levels
- Thyroid function tests
- Evaluation for diabetes or metabolic syndrome
Management
- Treat underlying hormonal disorder (e.g., testosterone replacement therapy, cabergoline for prolactinoma, thyroxine for hypothyroidism)
- Lifestyle changes (weight loss, exercise, stress management)
- Phosphodiesterase type 5 inhibitors (e.g., sildenafil) may help but are less effective if hormone imbalance persists
- Counseling or therapy if psychological overlay exists
When hormonal causes are identified and treated, erectile function and overall well-being can significantly improve.
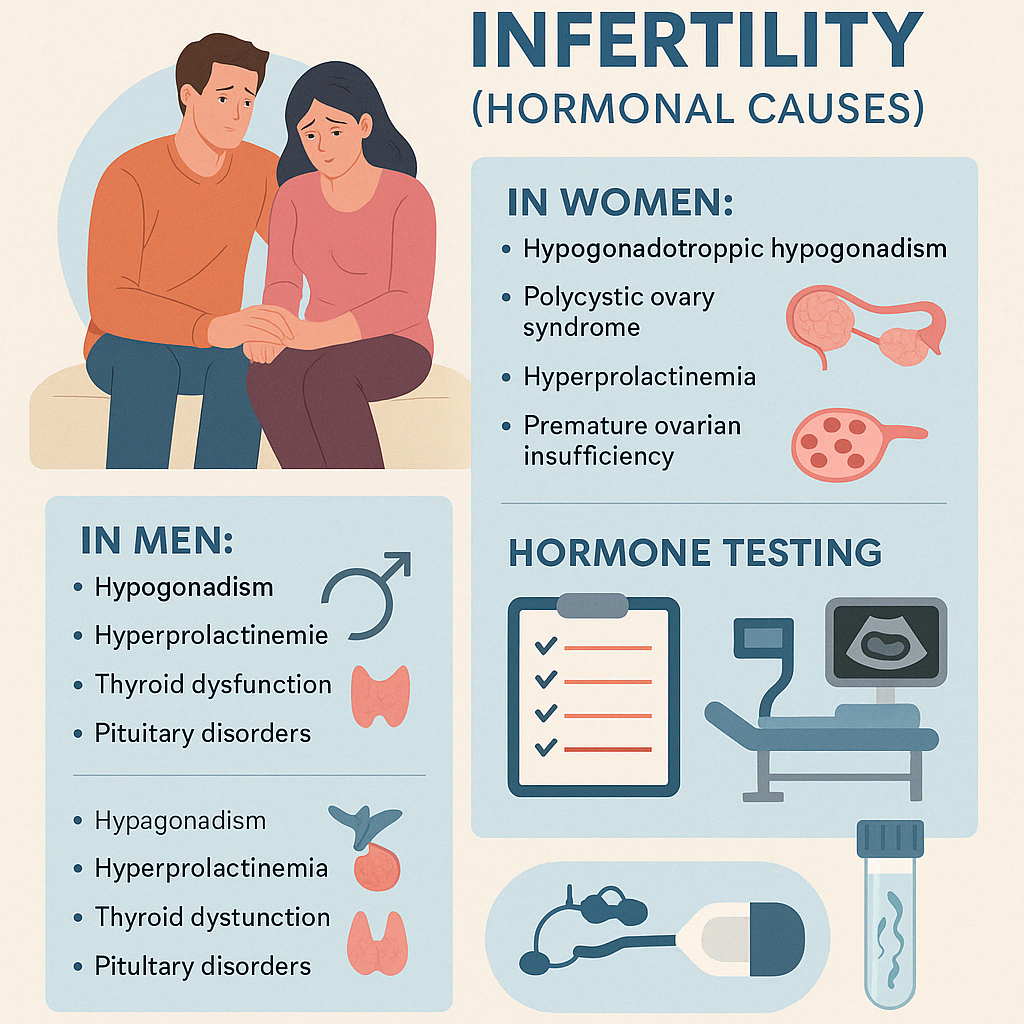
6. Infertility (hormonal causes)
Infertility is defined as the inability to conceive after one year of regular, unprotected intercourse. Hormonal causes play a significant role in both male and female infertility, often due to disruptions in the hypothalamic-pituitary-gonadal (HPG) axis.
In Women:
- Hypogonadotropic hypogonadism (low GnRH, LH, FSH) — may result from excessive exercise, stress, or pituitary disorders
- Polycystic Ovary Syndrome (PCOS) — causes chronic anovulation due to insulin resistance and hyperandrogenism
- Hyperprolactinemia — suppresses ovulation and menstrual regularity
- Premature Ovarian Insufficiency (POI) — results in depleted ovarian follicles and low estrogen
In Men:
- Hypogonadism — leads to low testosterone and reduced sperm production
- Hyperprolactinemia — impairs gonadotropin secretion
- Thyroid dysfunction — affects libido and spermatogenesis
- Kallmann syndrome or pituitary disorders — cause low FSH/LH and poor sperm production
Diagnosis
- Hormone testing: FSH, LH, prolactin, estradiol/testosterone, TSH
- Ovulation tracking and semen analysis
- Ultrasound or MRI to evaluate ovaries, uterus, or pituitary
Management
- Treat the underlying hormonal imbalance
- Ovulation induction (e.g., clomiphene, letrozole, gonadotropins) in women
- Testosterone replacement or gonadotropin therapy in men (note: exogenous testosterone suppresses sperm production)
- Assisted reproductive techniques (ART): IUI, IVF, or ICSI in select cases
With proper hormonal evaluation and therapy, many couples facing infertility can successfully conceive.