Parathyroid Gland Disorders
This group of endocrine diseases includes the following conditions
- Primary Hyperparathyroidism
- Secondary Hyperparathyroidism
- Tertiary Hyperparathyroidism
- Hypoparathyroidism
- Pseudohypoparathyroidism
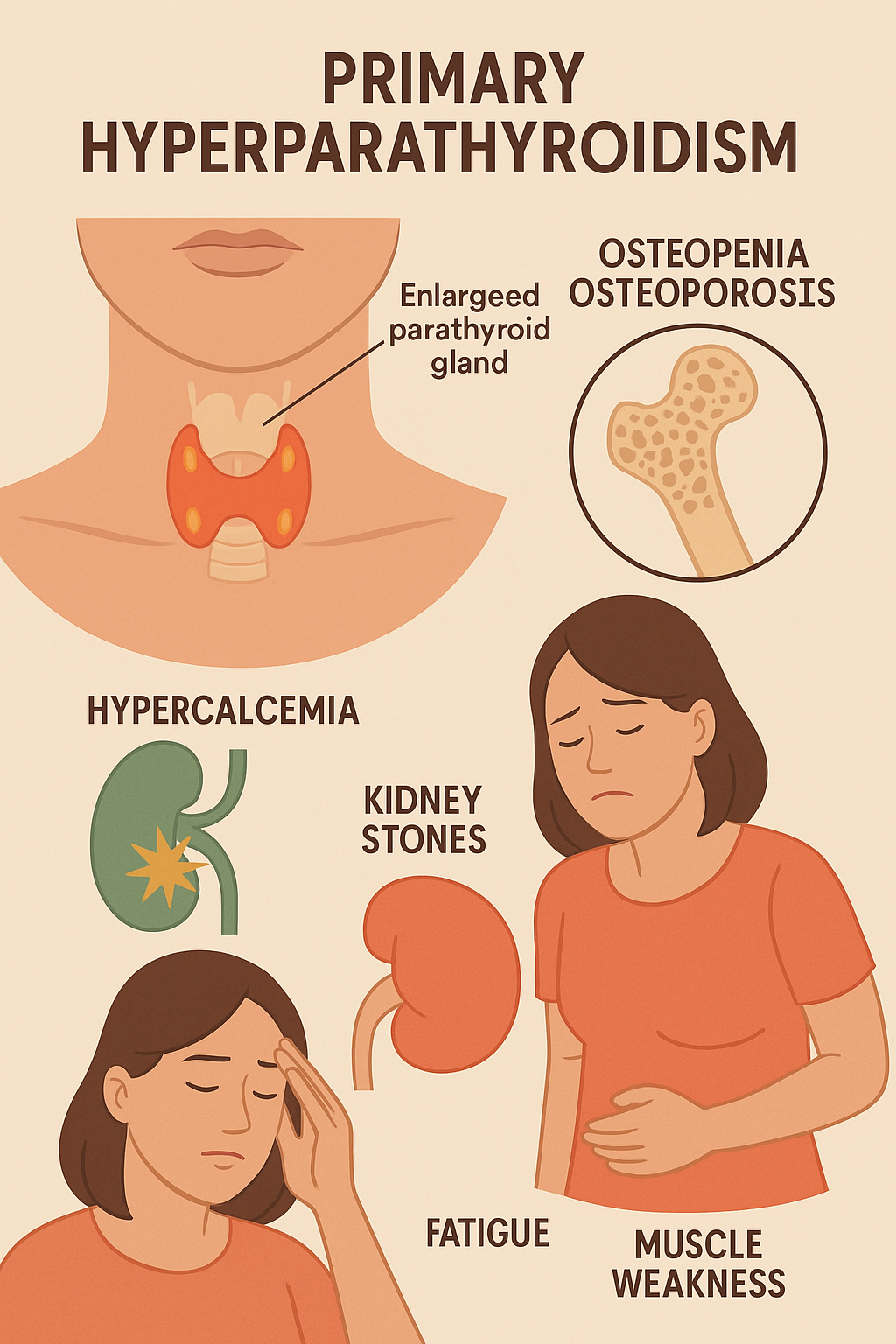
1. Primary Hyperparathyroidism
Primary Hyperparathyroidism (PHPT) is a condition in which one or more of the parathyroid glands secrete excessive amounts of parathyroid hormone (PTH), leading to elevated calcium levels in the blood (hypercalcemia). It is most commonly caused by a parathyroid adenoma, less commonly by parathyroid hyperplasia or carcinoma.
PTH plays a crucial role in maintaining calcium and phosphorus balance by acting on bones, kidneys, and the intestines. In PHPT, the persistently high levels of PTH cause bone resorption, increased calcium reabsorption by the kidneys, and increased intestinal absorption of calcium.
Many patients are asymptomatic and are diagnosed incidentally during routine blood tests showing high calcium levels. When symptoms do occur, they are often summarized by the mnemonic:
"Bones, Stones, Groans, and Psychiatric Overtones" — referring to:
- Bone pain, fractures, and osteoporosis
- Kidney stones and polyuria
- Abdominal pain, constipation, and pancreatitis
- Depression, fatigue, and memory issues
Long-standing PHPT can also lead to renal dysfunction, hypertension, and cardiac arrhythmias.
Diagnosis is confirmed by elevated serum calcium, high or inappropriately normal PTH, low serum phosphate, and elevated 24-hour urinary calcium. Bone density testing and imaging such as ultrasound or sestamibi scans help localize the affected gland(s).
Treatment is surgical — parathyroidectomy is the definitive cure. In mild or asymptomatic cases, monitoring may be considered. After surgery, calcium and vitamin D levels must be monitored closely.
With early detection and treatment, PHPT has an excellent prognosis and can prevent long- term complications.
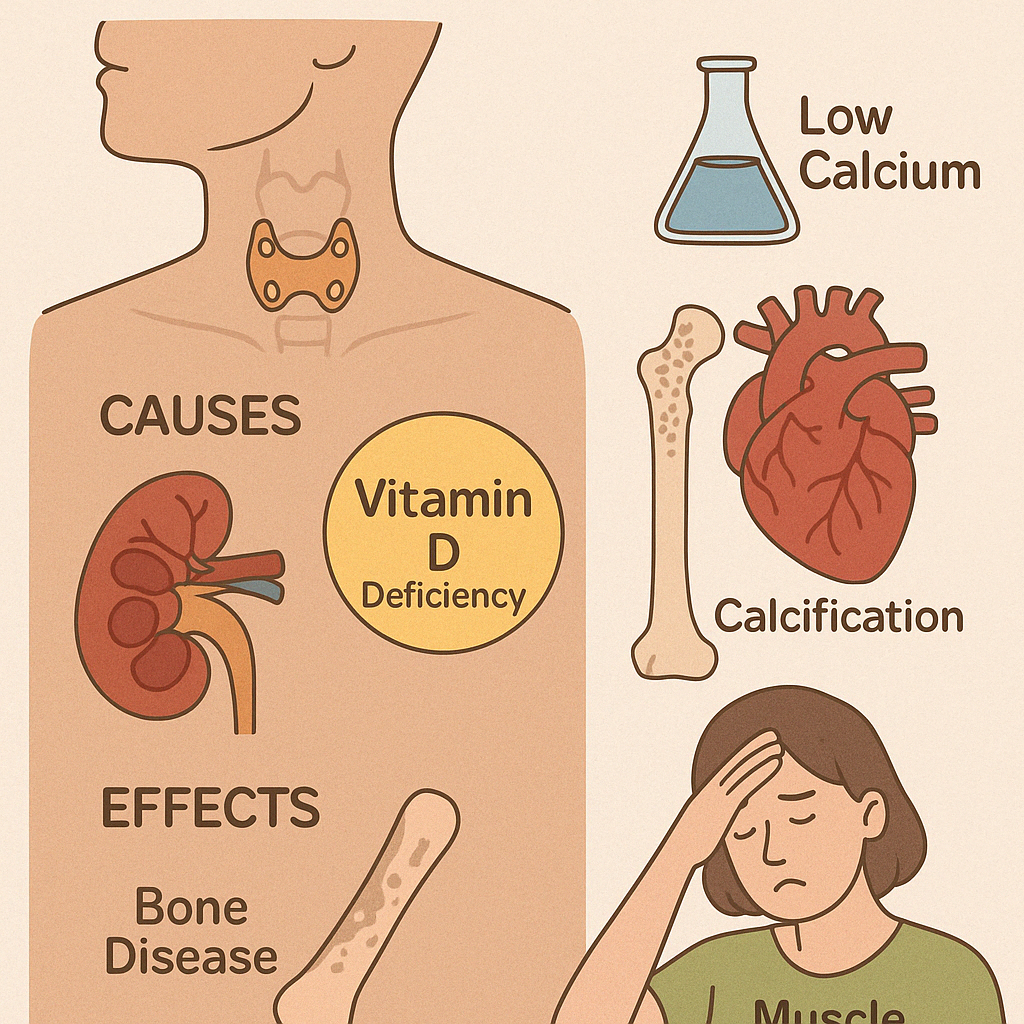
2. Secondary Hyperparathyroidism
Secondary Hyperparathyroidism is a condition characterized by excessive secretion of parathyroid hormone (PTH) as a compensatory response to chronic low calcium levels. Unlike primary hyperparathyroidism, the parathyroid glands are not inherently diseased — they are reacting to another underlying cause, most commonly chronic kidney disease (CKD) or vitamin D deficiency.
In chronic kidney disease, the kidneys fail to convert vitamin D into its active form and cannot excrete phosphate efficiently. This leads to low calcium and high phosphate levels in the blood, both of which stimulate the parathyroid glands to secrete more PTH. Over time, this persistent stimulation can cause the glands to enlarge and become overactive.
Clinical features may include:
- Bone pain and fractures (renal osteodystrophy)
- Muscle weakness and fatigue
- Vascular calcifications and cardiovascular complications
- Itching (pruritus)
- Skeletal deformities in children with CKD
Laboratory findings typically show low or normal calcium, high phosphate, elevated PTH, and low levels of active vitamin D.
Management includes:
- Phosphate binders to reduce phosphate absorption
- Vitamin D analogs or calcitriol to suppress PTH secretion
- Calcimimetics (e.g., cinacalcet) to trick the parathyroid gland into sensing normal calcium
- Dietary phosphate restriction
In severe or refractory cases, parathyroidectomy may be necessary.
Early diagnosis and targeted treatment can prevent bone deformities, vascular complications, and improve quality of life, especially in patients with long-standing kidney disease.
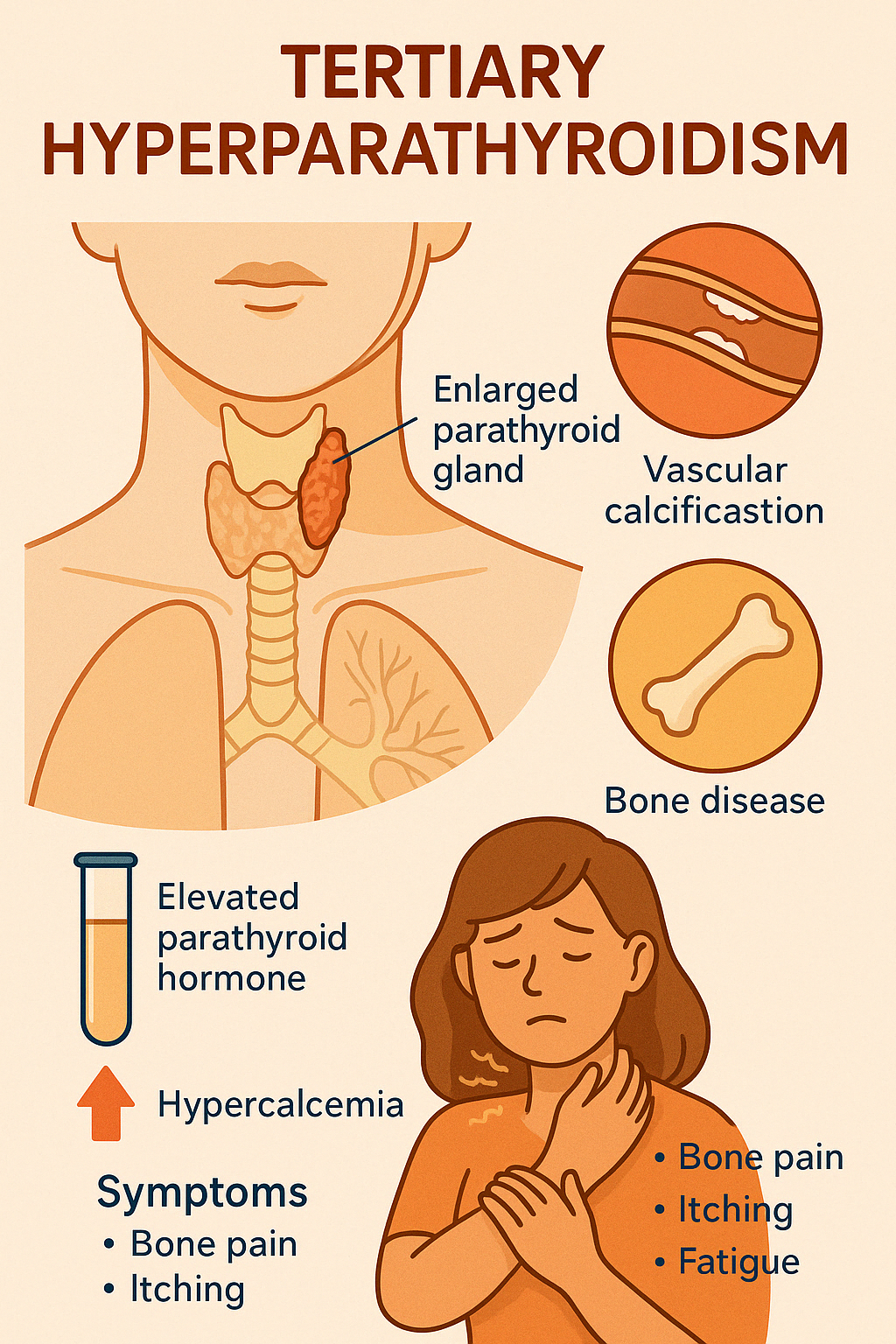
3. Tertiary Hyperparathyroidism
Tertiary Hyperparathyroidism is a condition that occurs almost exclusively in patients with chronic kidney disease (CKD), especially those on long-term dialysis or after renal transplantation. It develops when the parathyroid glands, after prolonged stimulation in secondary hyperparathyroidism, become autonomously overactive, secreting excess parathyroid hormone (PTH) even after the original trigger (like low calcium) is resolved.
This state represents the transition from a compensatory response to an independent disease process. The parathyroid glands often become hyperplastic or form nodules, resulting in persistently elevated PTH levels despite normal or even high serum calcium.
Common symptoms and complications include:
- Bone pain, fractures, and skeletal deformities
- Severe osteoporosis (renal osteodystrophy)
- Itching, fatigue, and muscle weakness
- Vascular and soft tissue calcifications
- Calciphylaxis is a life-threatening condition with painful skin ulcers due to calcium deposits in blood vessels
Laboratory findings show elevated PTH, hypercalcemia, and normal or high phosphate levels. Vitamin D levels may remain low due to impaired conversion in kidney disease.
Treatment typically involves:
- Medical therapy with phosphate binders, vitamin D analogs, and calcimimetics (e.g., cinacalcet)
- If medical therapy fails, subtotal or total parathyroidectomy is recommended
Early recognition and appropriate management are crucial to prevent severe bone and vascular complications and to improve long-term outcomes in patients with advanced kidney disease
Engage With Dr. Vipin Mishra
Whether you are dealing with chronic endocrine condition or just want to understand your body better, or wish to obtain an exalted consciousness, you can take help and guidance from Dr. Vipin Mishra.
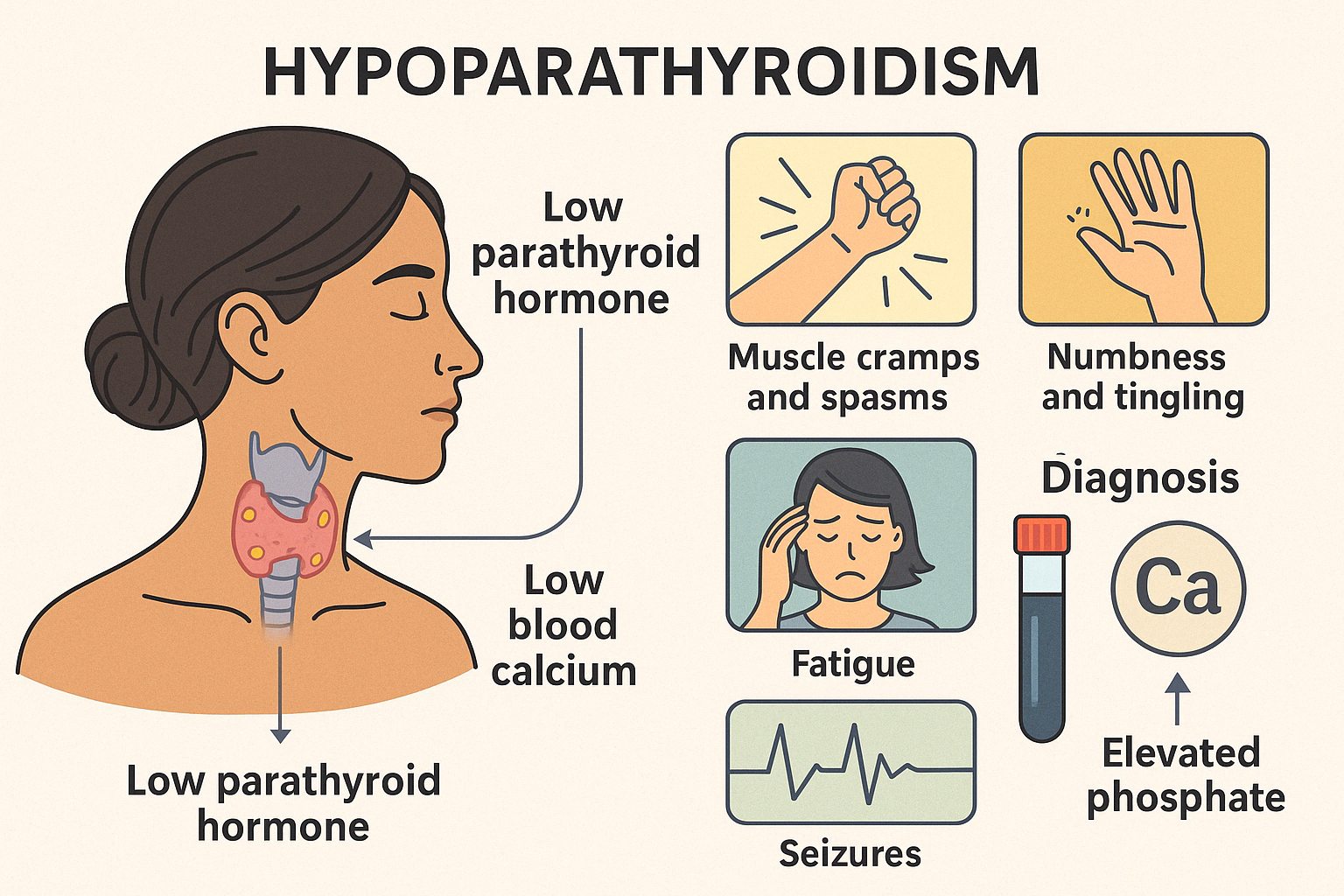
Engage With Dr. Vipin Mishra4. Hypoparathyroidism
Definition and Causes
Hypoparathyroidism is a rare endocrine disorder characterized by inadequate secretion of parathyroid hormone (PTH), resulting in low blood calcium (hypocalcemia) and high phosphate levels. The most common cause is accidental damage or removal of the parathyroid glands during thyroid or neck surgery. Other causes include autoimmune destruction, genetic syndromes (e.g., DiGeorge syndrome), or radiation therapy.
Clinical Presentation
The hallmark features stem from low calcium levels affecting nerves and muscles. Patients may present with:
- Muscle cramps and spasms (tetany)
- Numbness or tingling in fingers, toes, and around the mouth
- Seizures
- Fatigue, irritability, and anxiety
- Chvostek's and Trousseau's signs (clinical signs of neuromuscular irritability)
In chronic cases, dry skin, brittle nails, hair loss, dental defects, cataracts, and calcification in the brain may occur.
Diagnosis
It is diagnosed by low serum calcium, low or inappropriately normal PTH, and elevated phosphate levels. Vitamin D levels are also evaluated to rule out nutritional causes.
Management
Treatment includes oral calcium supplements, active vitamin D (calcitriol), and monitoring of serum calcium and phosphate. In severe cases, intravenous calcium may be needed. Recombinant PTH therapy is considered in select cases of chronic, difficult-to-manage hypoparathyroidism.
Prognosis
With careful long-term management and regular monitoring, most patients can maintain good quality of life and avoid complications.
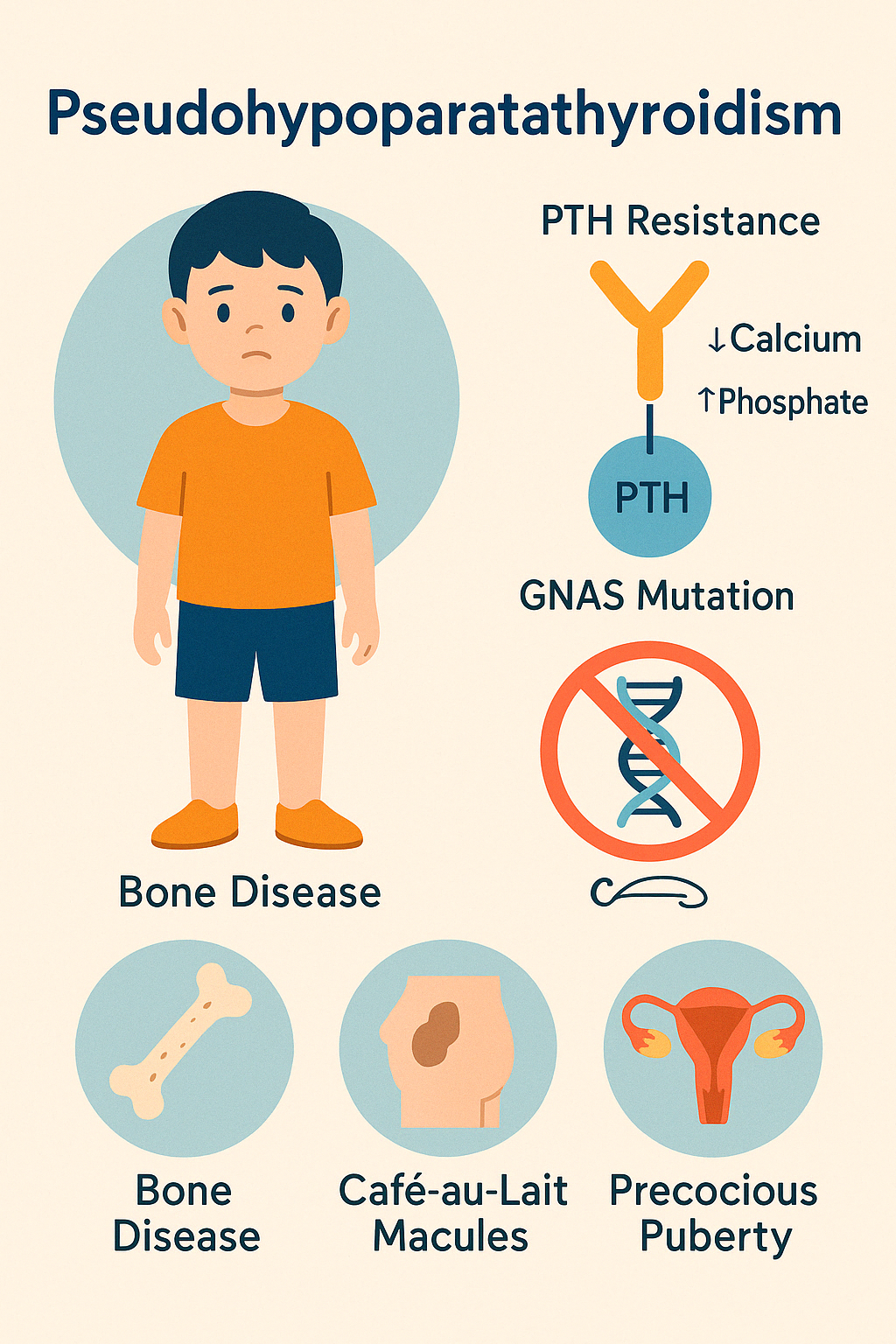
5. Pseudohypoparathyroidism
Pseudohypoparathyroidism (PHP) is a rare genetic disorder where the body is resistant to parathyroid hormone (PTH) despite having normal or elevated levels of the hormone. As a result, the physiological actions of PTH, especially its ability to maintain calcium and phosphate balance, are impaired, leading to low calcium and high phosphate levels in the blood, much like actual hypoparathyroidism.
The most well-known form is Type 1a, often associated with a condition called Albright Hereditary Osteodystrophy (AHO). Patients with AHO may have:
- Short stature
- Round face
- Obesity
- Subcutaneous calcifications
- Brachydactyly (shortened fourth and fifth fingers)
These skeletal features are often apparent early in life. Cognitive delay may also be present in some cases.
Other types of PHP may not show the physical features of AHO but still exhibit biochemical resistance to PTH. Rarely, resistance to other hormones (like TSH, gonadotropins) may also occur.
Laboratory findings include:
- Low serum calcium
- High phosphate
- Elevated or inappropriately normal PTH
Diagnosis is confirmed through biochemical tests and genetic testing (e.g., GNAS gene mutations).
Treatment is similar to hypoparathyroidism and includes oral calcium supplements, active vitamin D (calcitriol), and monitoring of calcium and phosphate levels. Careful growth and developmental monitoring is essential in pediatric cases.
With lifelong management and supportive care, most individuals with PHP can lead normal lives.