Calcium and Bone Disorders
This group of endocrine diseases includes the following conditions
- Hypercalcemia (non-parathyroid causes)
- Hypocalcemia (non-parathyroid causes)
- Vitamin D Deficiency and Osteomalacia
- Osteoporosis
- Paget's Disease of Bone
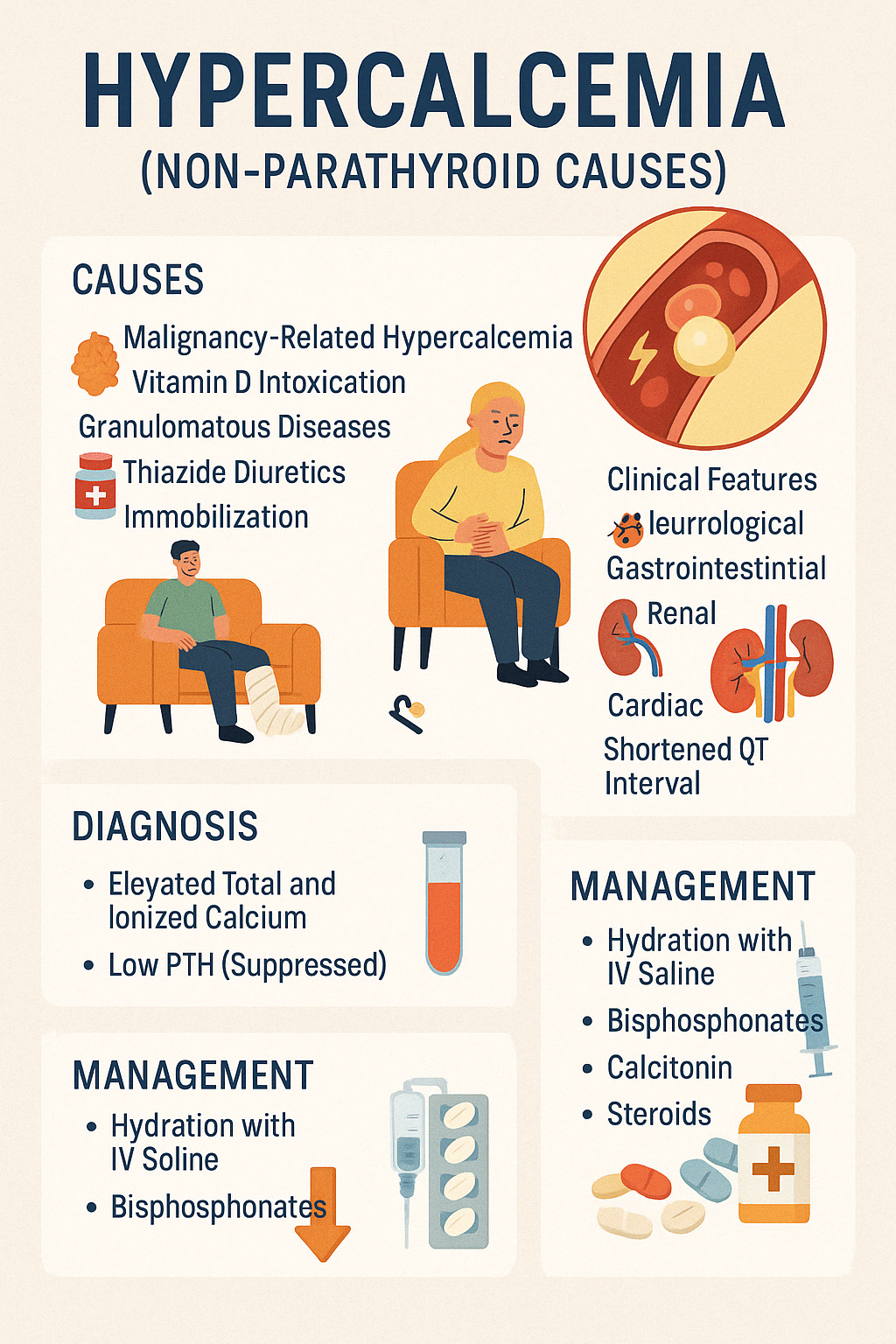
1. Hypercalcemia (non-parathyroid causes)
Hypercalcemia is defined as a serum calcium level >10.5 mg/dL. While primary hyperparathyroidism is the most common cause in outpatients, non-parathyroid causes are more common in hospitalized patients and can be serious or life-threatening.
Major Non-Parathyroid Causes:
- Malignancy-related hypercalcemia
- Most common in hospitalized patients
- Due to secretion of PTH-related peptide (PTHrP), bone metastases, or calcitriol overproduction
- Vitamin D intoxication
- Granulomatous diseases (e.g., sarcoidosis, tuberculosis — macrophages increase 1-alpha hydroxylase activity)
- Thiazide diuretics (reduce renal calcium excretion)
- Immobilization (especially in adolescents or those with high bone turnover)
- Endocrine disorders: hyperthyroidism, adrenal insufficiency
- Milk-alkali syndrome
Clinical Features:
- Neurological: fatigue, confusion, depression, coma (in severe cases)
- Gastrointestinal: nausea, vomiting, constipation, abdominal pain
- Renal: polyuria, polydipsia, nephrolithiasis, nephrocalcinosis
- Cardiac: hypertension, arrhythmias, shortened QT interval
Diagnosis:
- Elevated total and ionized calcium
- Low PTH (suppressed)
- Check PTHrP, vitamin D levels, serum/urine protein electrophoresis, TSH, and imaging for malignancy or granulomas
Management:
- Hydration with IV saline
- Bisphosphonates (e.g., zoledronic acid)
- Calcitonin for rapid effect
- Steroids (for vitamin D–mediated causes)
- Dialysis in severe, refractory cases
Identifying the underlying cause is critical for targeted management and preventing recurrence.
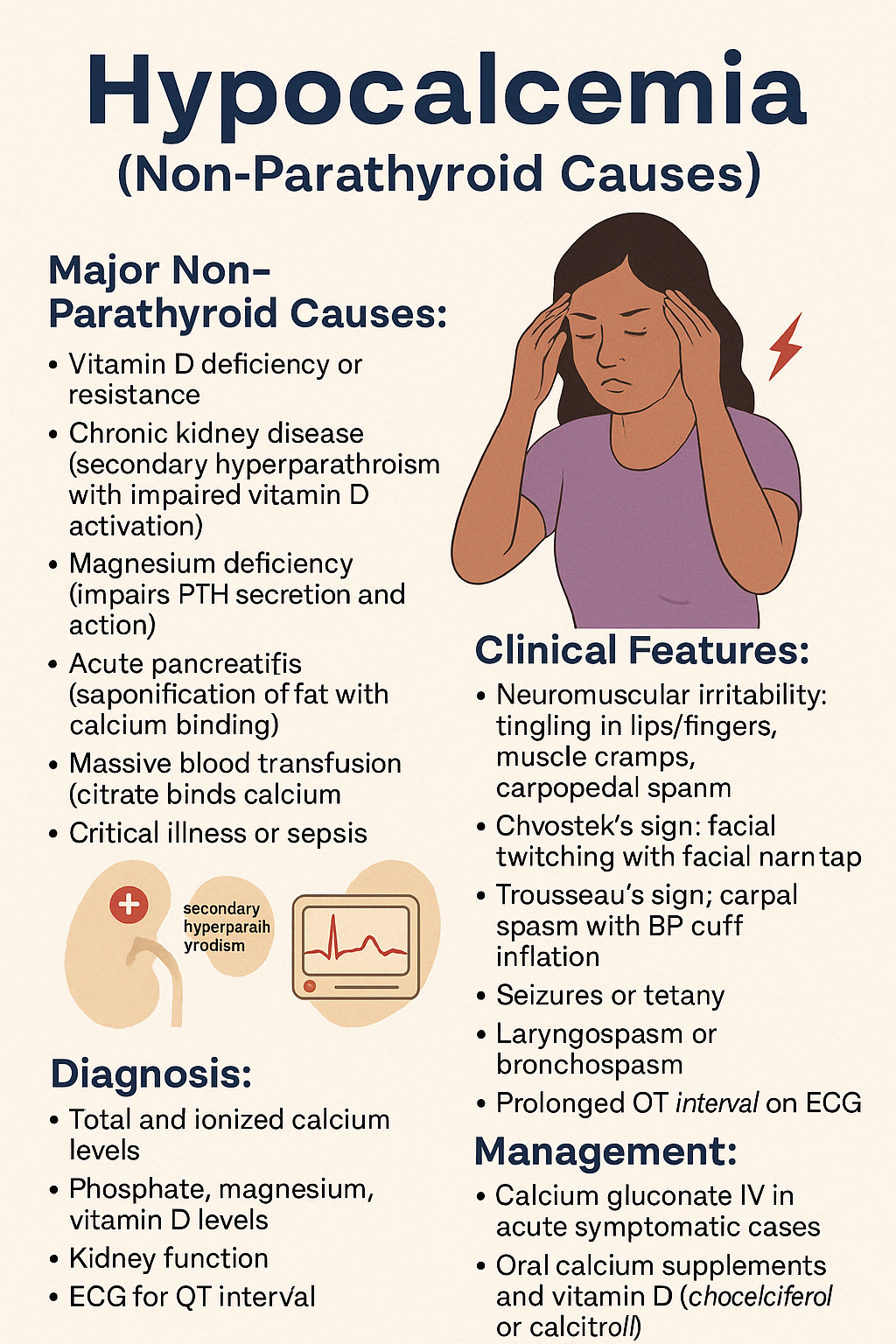
2. Hypocalcemia (non-parathyroid causes)
Hypocalcemia is defined as a serum calcium level below 8.5 mg/dL. While hypoparathyroidism is a major cause, many non-parathyroid etiologies contribute significantly and require prompt identification and management.
Major Non-Parathyroid Causes:
- Vitamin D deficiency or resistance
- Chronic kidney disease (secondary hyperparathyroidism with impaired vitamin D activation)
- Magnesium deficiency (impairs PTH secretion and action)
- Acute pancreatitis (saponification of fat with calcium binding)
- Massive blood transfusion (citrate binds calcium)
- Critical illness or sepsis
- Drugs: bisphosphonates, loop diuretics, chemotherapy agents
- Hypoalbuminemia (causes low total calcium; ionized calcium may be normal)
Clinical Features:
- Neuromuscular irritability: tingling in lips/fingers, muscle cramps, carpopedal spasm
- Chvostek's sign: facial twitching with facial nerve tap
- Trousseau's sign: carpal spasm with BP cuff inflation
- Seizures or tetany in severe cases
- Laryngospasm or bronchospasm
- Prolonged QT interval on ECG
Diagnosis:
- Total and ionized calcium levels
- Phosphate, magnesium, vitamin D levels
- Kidney function
- ECG for QT interval
- Exclude hypoalbuminemia (adjust calcium for albumin if needed)
Management:
- Calcium gluconate IV in acute symptomatic cases
- Oral calcium supplements and vitamin D (cholecalciferol or calcitriol)
- Magnesium replacement if deficient
- Address underlying causes (e.g., stop offending drugs, treat CKD or pancreatitis)
Prompt correction prevents life-threatening complications and improves neuromuscular and cardiac stability.
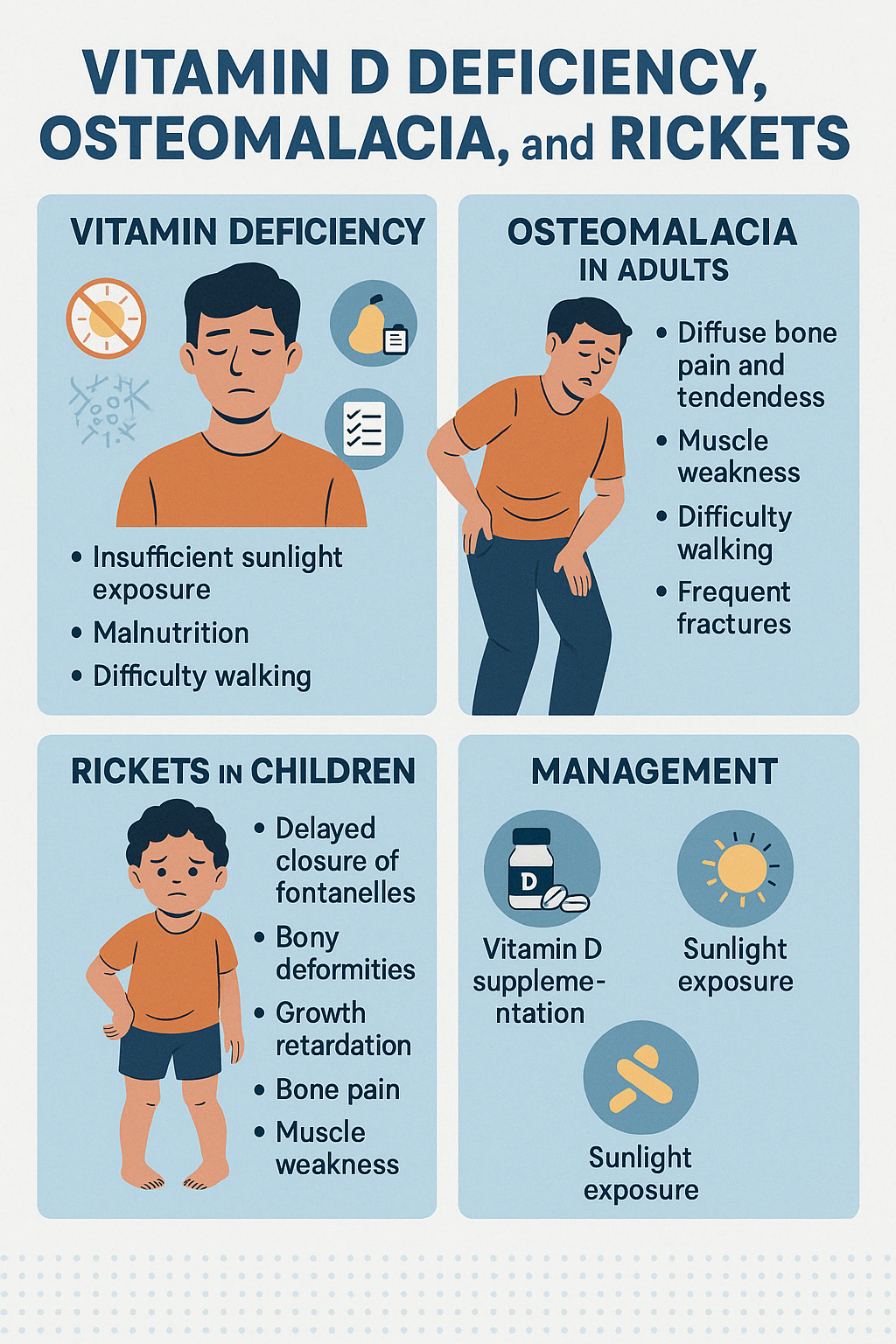
3. Vitamin D Deficiency and Osteomalacia
Vitamin D Deficiency
Vitamin D plays a crucial role in calcium and phosphate absorption, bone mineralization, and immune modulation. Deficiency arises from insufficient sunlight exposure, malnutrition, malabsorption syndromes, chronic kidney or liver disease, or certain medications (e.g., anticonvulsants).
Osteomalacia (in adults)
Osteomalacia refers to softening of bones due to defective mineralization of the bone matrix, usually resulting from vitamin D deficiency in adults.
Clinical Features:
- Diffuse bone pain and tenderness
- Muscle weakness (especially proximal muscles)
- Difficulty walking, waddling gait
- Frequent falls or fractures (especially ribs, vertebrae, femoral neck)
Investigations:
- Low serum vitamin D
- Low/normal calcium and phosphate
- Elevated alkaline phosphatase (ALP)
- Low urinary calcium
- X-rays: Looser's zones (pseudofractures)
Rickets (in children)
Rickets is the pediatric equivalent of osteomalacia and results in defective bone growth and skeletal deformities due to vitamin D deficiency during growth years.
Clinical Features:
- Delayed closure of fontanelles
- Frontal bossing and widening of wrists
- Bow legs (genu varum) or knock knees (genu valgum)
- Rachitic rosary (costochondral junction swelling)
- Delayed dentition and short stature
- Irritability, poor feeding
Investigations:
- Similar to osteomalacia
- X-rays show metaphyseal cupping and fraying
Management for Both:
- Vitamin D supplementation (cholecalciferol or ergocalciferol)
- Calcium supplements if deficient
- Sunlight exposure
- Treat underlying malabsorption or renal disorders if present
Prevention through early detection and supplementation is vital, especially in at-risk populations like exclusively breastfed infants, the elderly, or those with limited sun exposure.
Engage With Dr. Vipin Mishra
Whether you are dealing with chronic endocrine condition or just want to understand your body better, or wish to obtain an exalted consciousness, you can take help and guidance from Dr. Vipin Mishra.
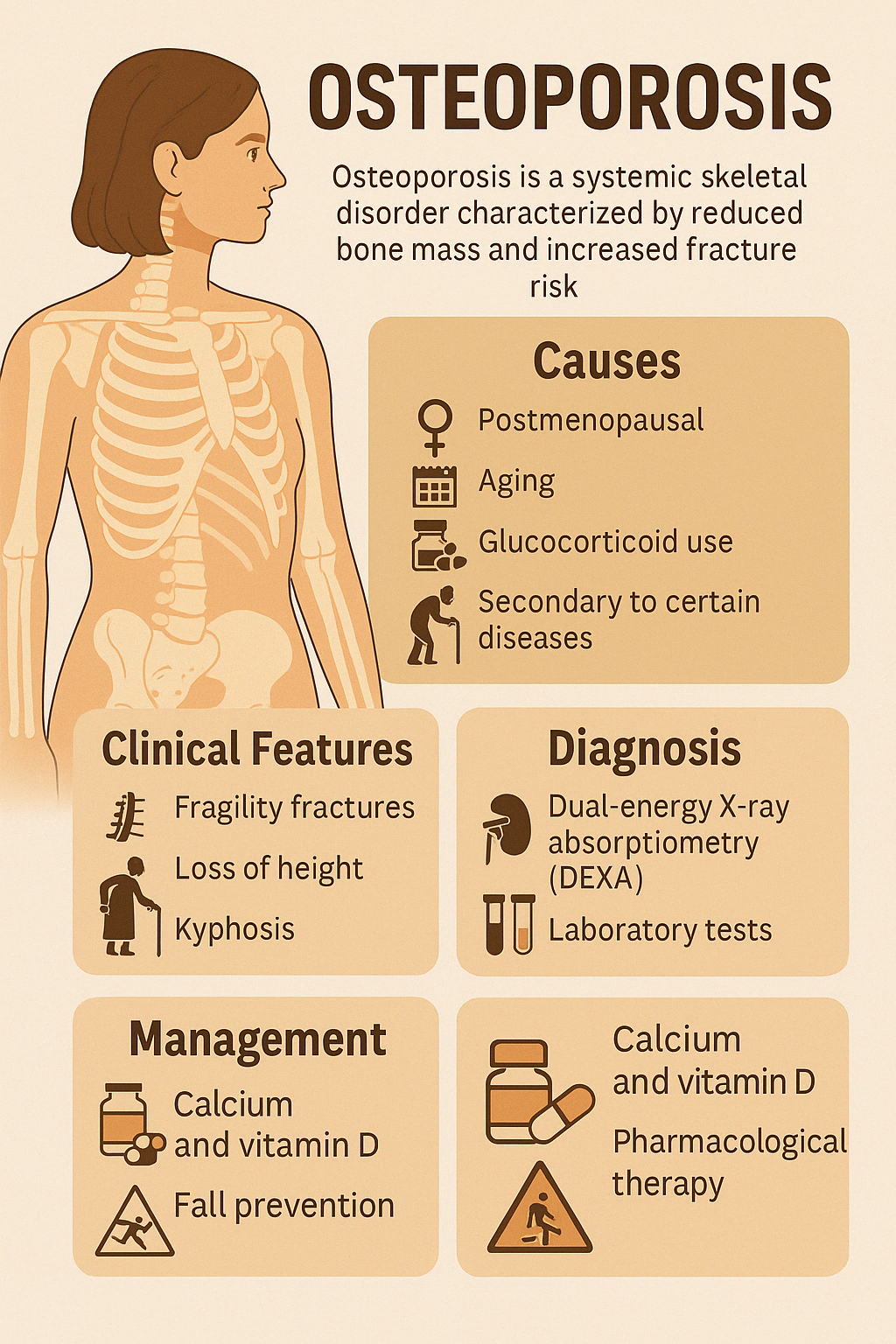
Engage With Dr. Vipin Mishra4. Osteoporosis
Osteoporosis is a systemic skeletal disorder characterized by reduced bone mass and microarchitectural deterioration, leading to increased bone fragility and fracture risk. It is most common in postmenopausal women and the elderly, but can affect both sexes and all age groups under specific conditions.
Causes:
Primary Osteoporosis:
- Postmenopausal (due to estrogen deficiency)
- Senile (age-related bone loss)
Secondary Osteoporosis:
- Glucocorticoid use
- Hyperthyroidism, hyperparathyroidism
- Chronic kidney or liver disease
- Malabsorption syndromes (e.g., celiac disease)
- Hypogonadism
- Rheumatologic conditions, immobilization, alcoholism
Clinical Features:
- Often asymptomatic until a fracture occurs
- Fragility fractures: vertebrae (compression), hip, distal radius (Colles')
- Loss of height, kyphosis, and back pain
- Increased risk of falls and associated complications
Diagnosis:
- Dual-energy X-ray absorptiometry (DEXA) scan is the gold standard
- T-score ≤ –2.5 indicates osteoporosis
- Labs to rule out secondary causes: calcium, phosphate, ALP, PTH, vitamin D, TSH
Management:
Lifestyle Measures:
- Weight-bearing exercise
- Smoking cessation and moderation of alcohol
- Fall prevention strategies
Supplementation:
- Calcium (1000–1200 mg/day)
- Vitamin D (800–1000 IU/day)
Pharmacological:
- Bisphosphonates (alendronate, risedronate)
- Denosumab
- Teriparatide (anabolic therapy for severe cases)
- Raloxifene, HRT in select cases
Early diagnosis and proactive treatment can dramatically reduce fracture risk and improve long- term outcomes.
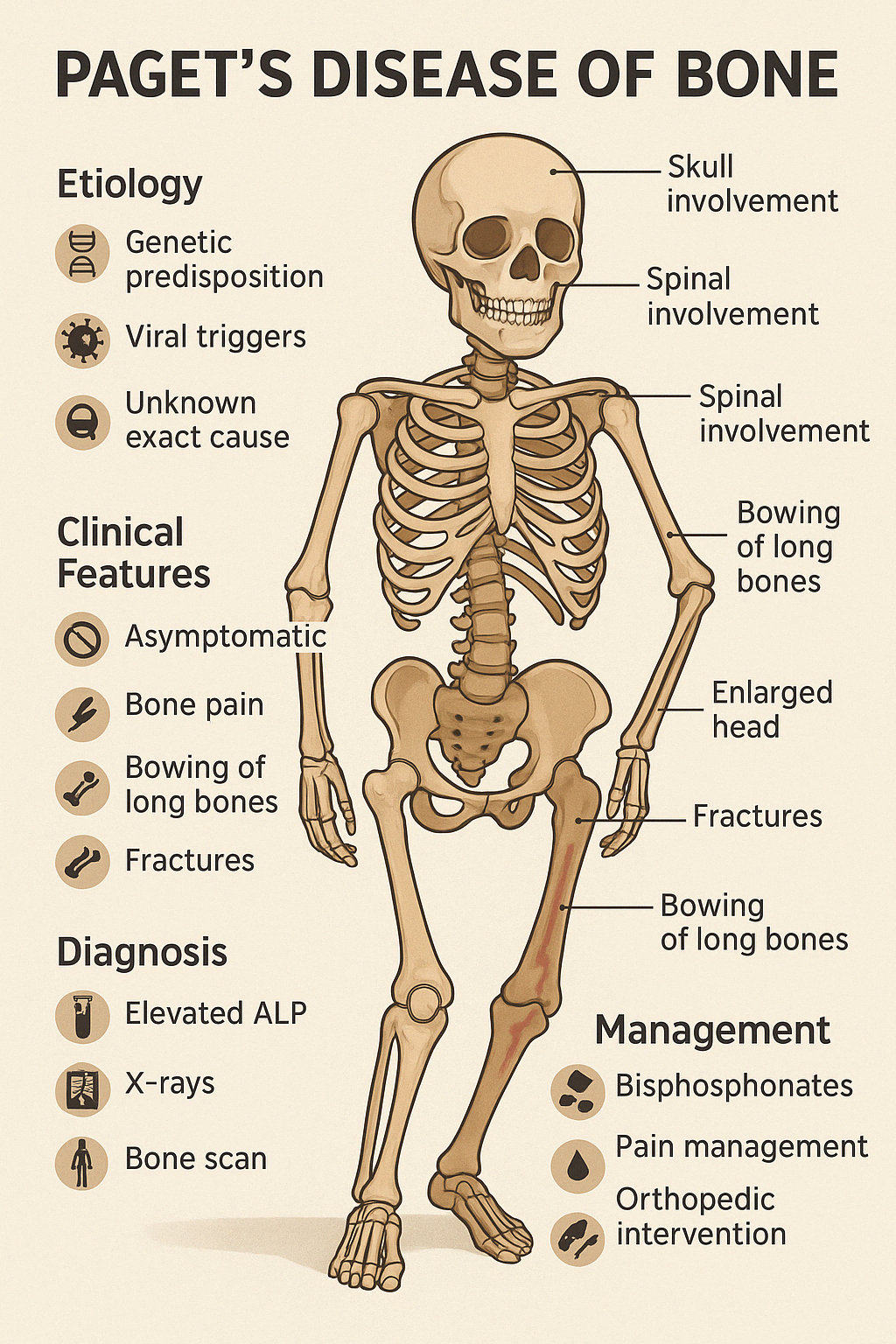
5. Paget’s Disease of Bone
Paget’s Disease of Bone is a chronic skeletal disorder characterized by abnormal bone remodeling, where excessive bone resorption is followed by disorganized and structurally weak bone formation. It most commonly affects the pelvis, spine, skull, femur, and tibia.
The condition usually affects people over the age of 50 and may involve one or multiple bones (monostotic or polyostotic).
Etiology:
- Exact cause unknown
- Possible genetic predisposition (e.g., SQSTM1 mutation)
- Viral triggers (e.g., paramyxovirus) have been suggested
Clinical Features:
- Often asymptomatic, discovered incidentally by elevated ALP or imaging
- Bone pain is the most common symptom
- Bowing of long bones (especially in the legs)
- Fractures, especially in weight-bearing bones
- Skull involvement: enlarged head, hearing loss, tinnitus
- Spinal involvement: nerve compression, back pain
- Warmth over affected bones due to hypervascularity
Diagnosis:
- Elevated serum alkaline phosphatase (ALP)
- Normal calcium and phosphate levels
- X-rays: cortical thickening, lytic and sclerotic lesions
- Bone scan to assess extent of disease
Complications:
- Fractures and deformities
- Osteoarthritis in adjacent joints
- Neurological complications (e.g., deafness, radiculopathy)
- Rarely, transformation into osteosarcoma
Management:
- Bisphosphonates (e.g., zoledronic acid) are first-line therapy
- Pain management with NSAIDs
- Orthopedic interventions for fractures or deformities
- Monitoring of ALP and symptoms during follow-up
Early treatment can reduce symptoms, control disease progression, and improve quality of life.