Growth Disorders
This group of endocrine diseases includes the following conditions
- Growth Hormone Deficiency (GHD)
- Growth Hormone Excess (Acromegaly / Gigantism)
- Short Stature (non-GHD causes)
- Tall Stature (non-GH causes)
- Constitutional Growth Delay
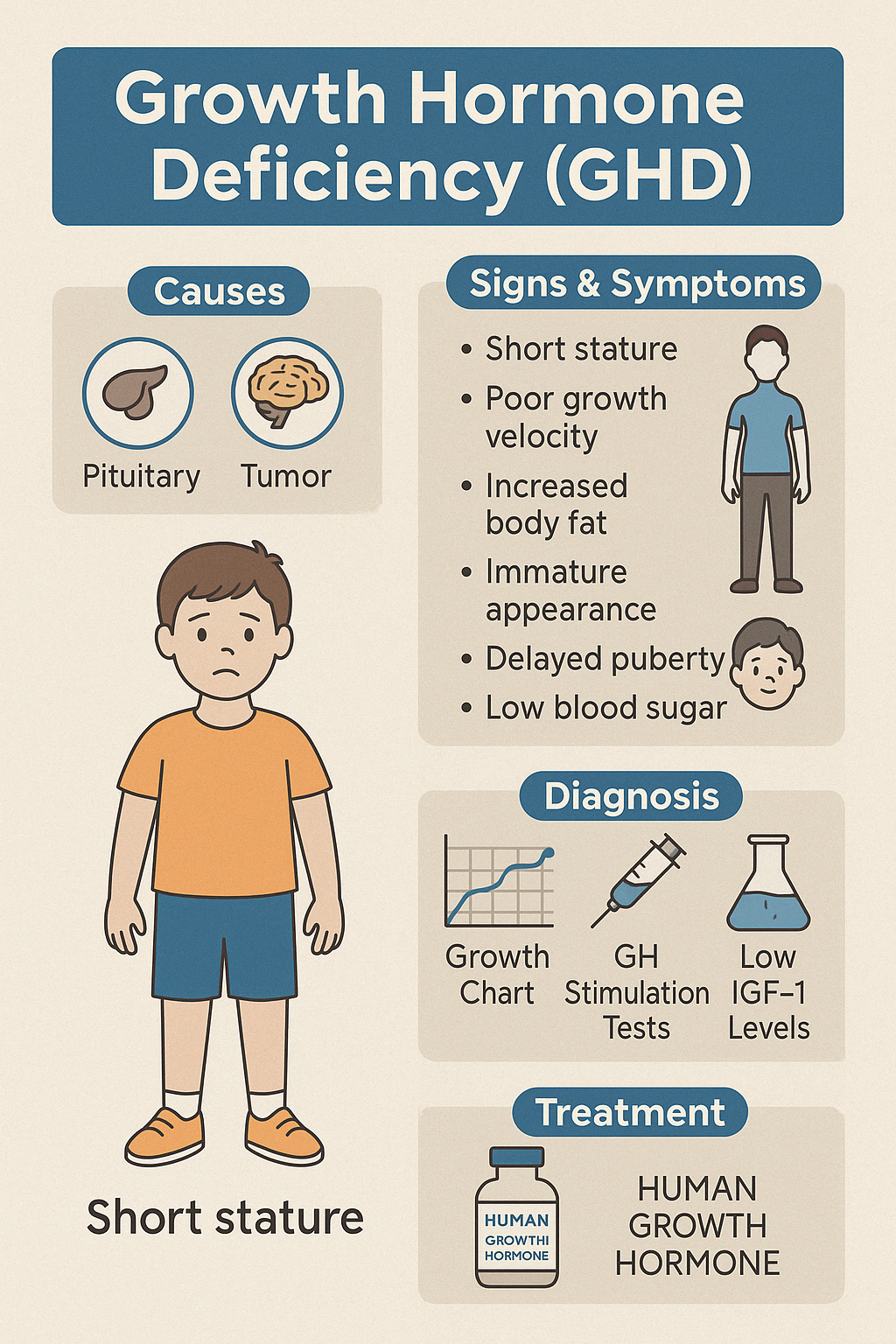
1. Growth Hormone Deficiency (GHD)
Growth Hormone Deficiency (GHD) is a condition in which the pituitary gland fails to produce enough growth hormone (GH), leading to impaired linear growth in children and various metabolic consequences in adults. It may be congenital or acquired later in life due to tumors, trauma, surgery, or radiation.
In Children:
- GHD typically presents as short stature with poor linear growth velocity, despite normal body proportions. Other signs may include:
- Increased body fat (especially around the waist)
- Immature facial features
- Delayed tooth eruption
- Delayed puberty
- Low blood sugar (in infants)
In Adults:
- GHD may cause:
- Decreased muscle mass and strength
- Increased fat accumulation
- Fatigue and low energy
- Impaired concentration and mood
- Osteopenia or osteoporosis
- Reduced exercise capacity
Diagnosis:
- Since GH is secreted in pulses, random GH measurements are unreliable. Diagnosis relies on:
- Growth charts and velocity tracking (in children)
- GH stimulation tests (e.g., insulin tolerance test, clonidine, arginine)
- Low IGF-1 levels
- Pituitary MRI to identify structural abnormalities or lesions
Treatment:
- Daily recombinant human growth hormone (rhGH) injections are the mainstay of therapy. Treatment in children improves final adult height, while adults benefit from improved body composition, energy levels, and quality of life.
Early diagnosis and proper management can profoundly improve long-term outcomes and development in children and restore metabolic health in adults
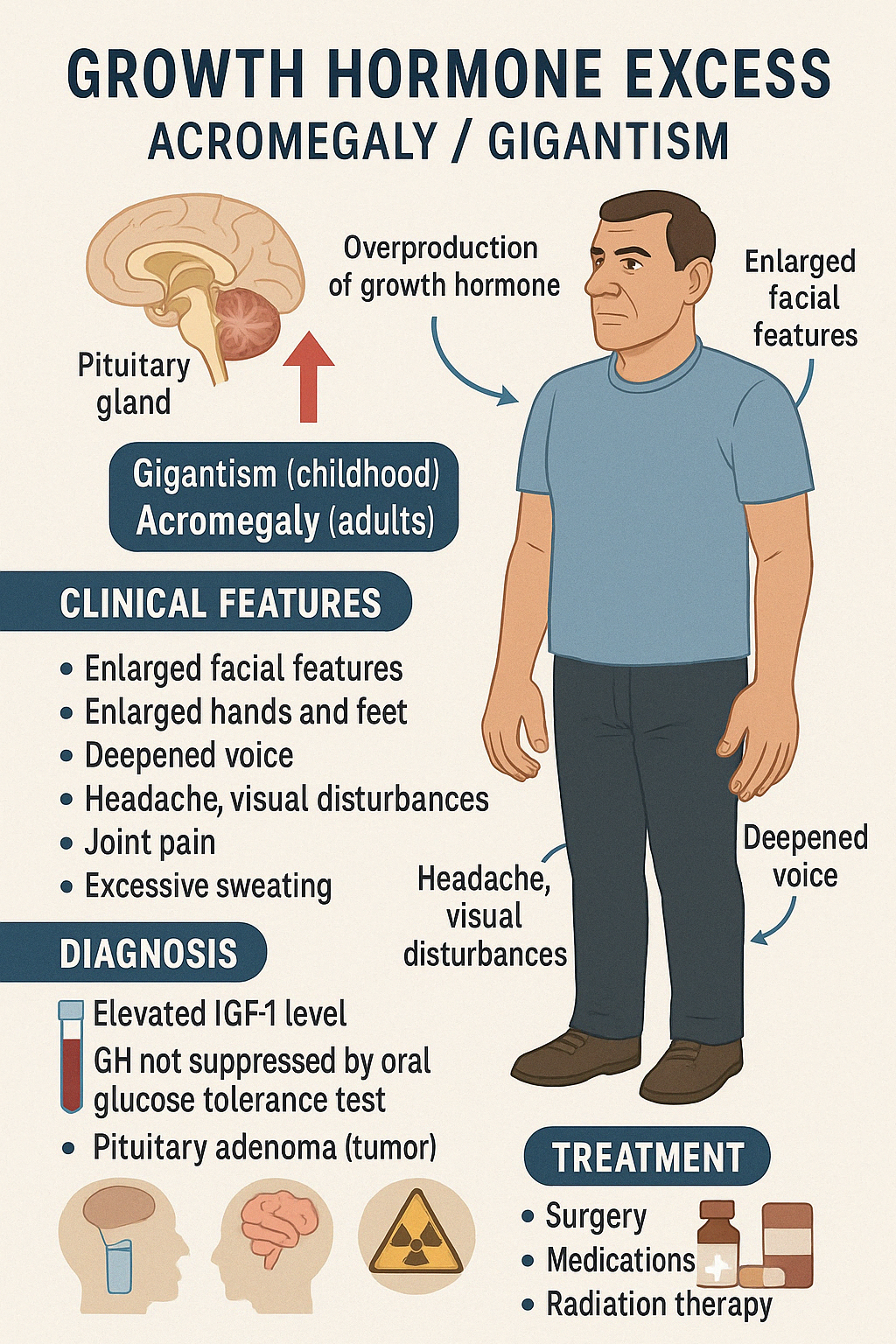
2. Growth Hormone Excess (Acromegaly / Gigantism)
Growth Hormone Excess is a rare hormonal disorder caused by overproduction of growth hormone (GH), usually due to a GH-secreting pituitary adenoma. The condition manifests differently depending on the age of onset:
- Gigantism occurs when GH excess starts before epiphyseal closure in childhood or adolescence, resulting in excessive linear growth and very tall stature.
- Acromegaly occurs in adults, after epiphyseal fusion, leading to thickening of bones and soft tissues rather than increased height.
Clinical Features
- In Gigantism (children):
- Abnormally tall stature
- Rapid and disproportionate growth
- Delayed puberty
- In Acromegaly (adults):
- Enlarged hands and feet (ring/shoe size increases)
- Coarse facial features (protruding jaw, enlarged nose and lips)
- Deepened voice
- Excessive sweating and oily skin
- Joint pain and arthritis
- Headaches and visual disturbances (from tumor compression)
- Menstrual irregularities or erectile dysfunction
- Insulin resistance and diabetes
- Hypertension and cardiomyopathy
Diagnosis
- Elevated IGF-1 levels
- Failure to suppress GH in oral glucose tolerance test (OGTT)
- MRI of the pituitary to identify adenoma
Treatment
- Transsphenoidal surgical removal of the pituitary tumor
- Medical therapy with somatostatin analogs (e.g., octreotide), GH receptor antagonists, or dopamine agonists
- Radiation therapy if surgery or medications are inadequate
Early diagnosis and treatment are crucial to prevent severe systemic complications and improve quality of life.
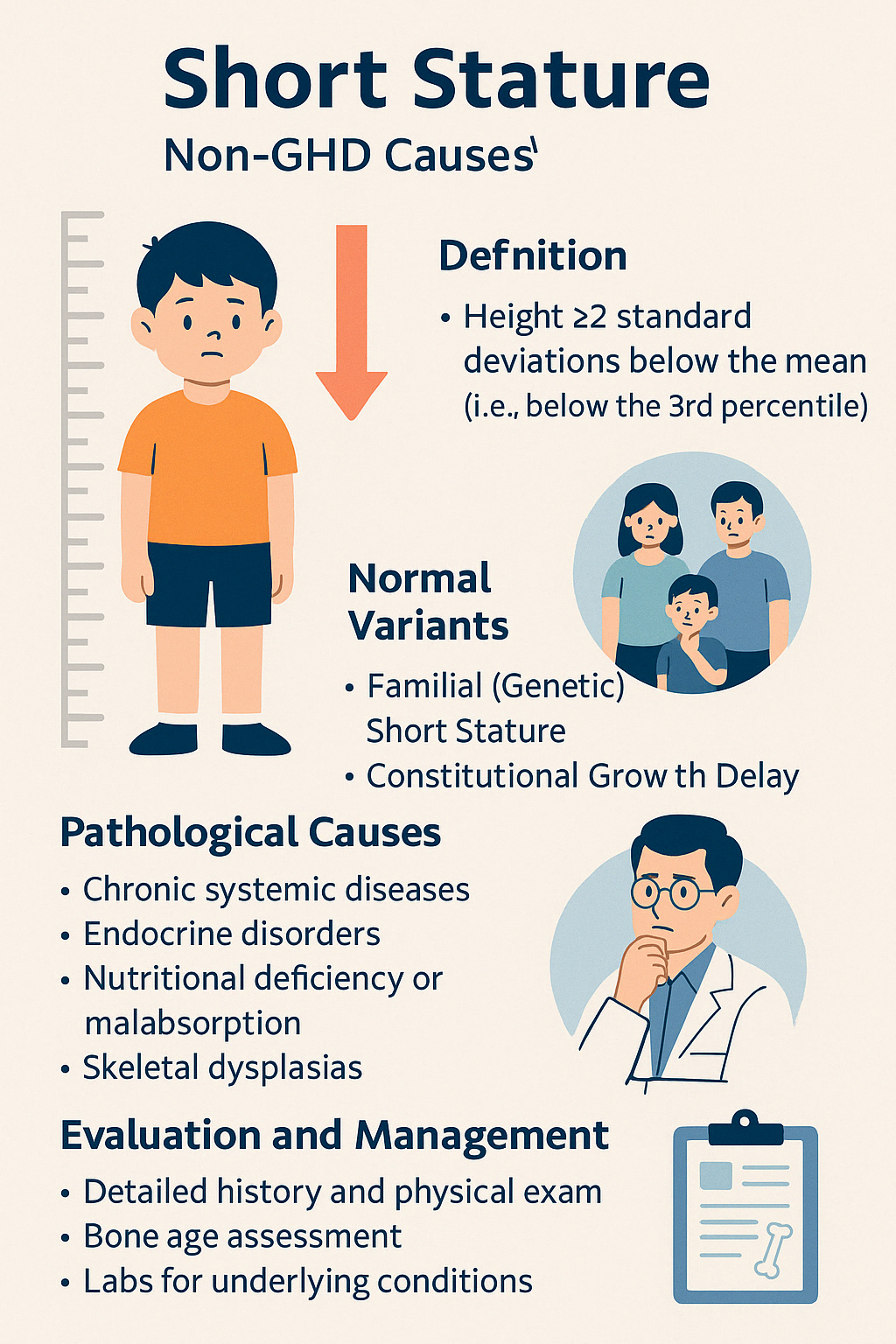
3. Short Stature (non-GHD causes)
Short stature is defined as height more than 2 standard deviations below the mean for age and sex (i.e., below the 3rd percentile). While Growth Hormone Deficiency (GHD) is one possible cause, many children with short stature have non-GHD etiologies — either normal variants or pathological conditions.
Normal Variants:
- Familial (Genetic) Short Stature
- Child is short but follows a consistent growth curve
- Parents are also short
- Bone age is consistent with chronological age
- Constitutional Growth Delay (see next topic)
- Slower growth but normal adult height
- Delayed bone age and puberty
Pathological Causes:
- Chronic systemic diseases (renal, cardiac, GI, or respiratory conditions)
- Endocrine disorders (hypothyroidism, Cushing's syndrome, poorly controlled diabetes)
- Nutritional deficiency or malabsorption (e.g., celiac disease)
- Skeletal dysplasias (e.g., achondroplasia)
- Psychosocial deprivation or emotional stress
Clinical Evaluation:
- Detailed history (birth, nutrition, family growth patterns)
- Growth charting and velocity analysis
- Bone age X-ray
- Screening labs for systemic and endocrine disease
- Karyotype in girls (to rule out Turner syndrome)
Management:
- Treat underlying cause, if identified
- Nutritional rehabilitation where applicable
- Hormonal therapy (e.g., thyroxine for hypothyroidism)
- Growth hormone therapy only in selected non-GHD conditions (e.g., Turner syndrome, SGA children)
Early identification and a structured diagnostic approach ensure optimal growth outcomes and help differentiate benign from serious causes.
Engage With Dr. Vipin Mishra
Whether you are dealing with chronic endocrine condition or just want to understand your body better, or wish to obtain an exalted consciousness, you can take help and guidance from Dr. Vipin Mishra.
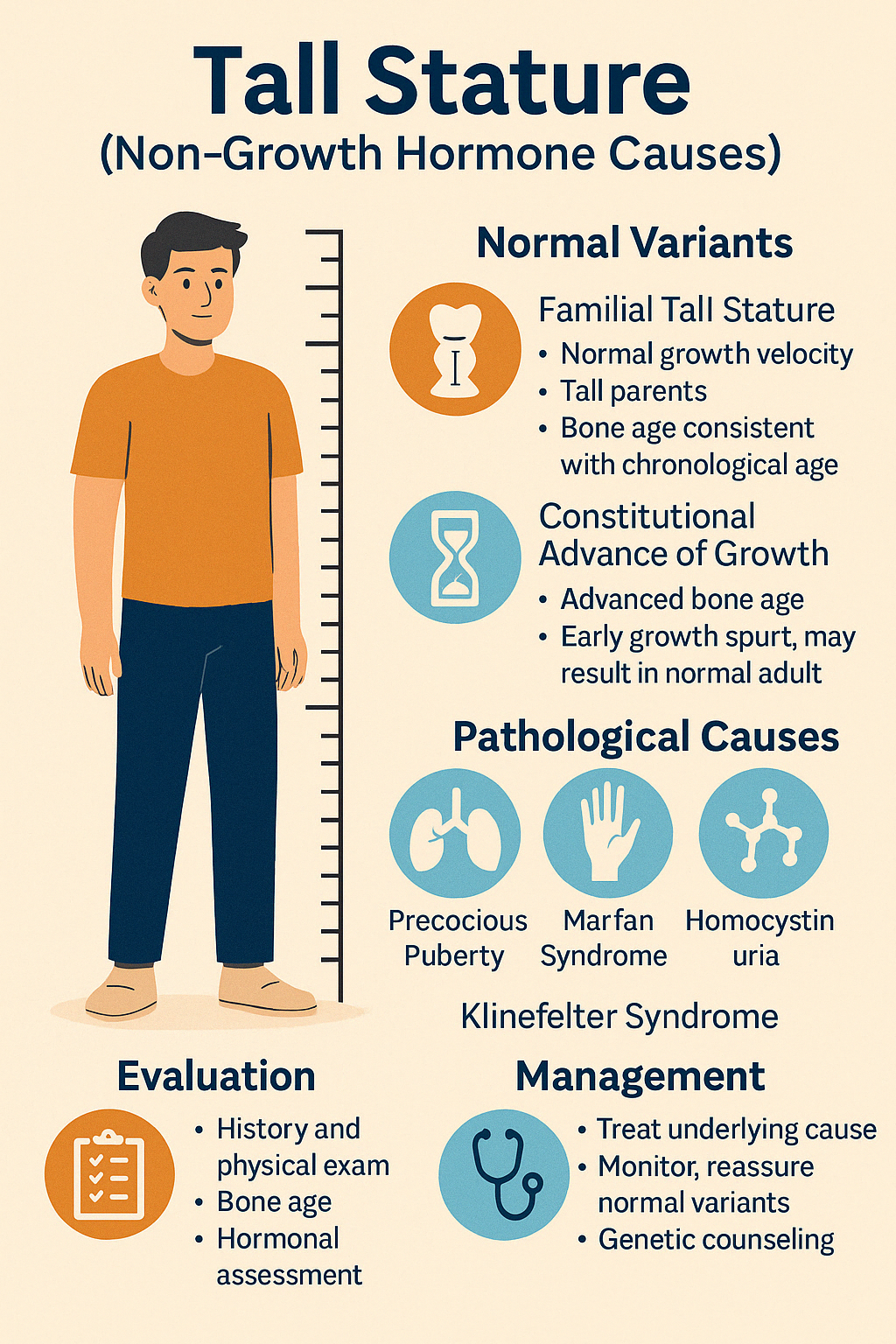
Schedule a Consultation4. Tall Stature (non-GH causes)
Tall stature is defined as a height greater than 2 standard deviations above the mean for age and sex (i.e., above the 97th percentile). While some children are simply tall due to familial traits, others may have underlying endocrine, genetic, or syndromic conditions that warrant evaluation.
Normal Variants:
- Familial Tall Stature
- Normal growth velocity
- Tall parents
- Bone age consistent with chronological age
- Constitutional Advance of Growth
- Advanced bone age
- Early growth spurt, may result in normal adult height
Pathological Causes:
- Precocious puberty (initial tall stature, early epiphyseal closure → short adult height)
- Hyperthyroidism
- Marfan syndrome (tall, thin body, long limbs, lens dislocation, aortic root dilation)
- Homocystinuria (resembles Marfan but with intellectual disability, thromboembolic risk)
- Klinefelter syndrome (tall males with small testes and infertility)
- Sotos syndrome (cerebral gigantism, developmental delay)
Evaluation:
- Detailed history (growth chart, family heights)
- Physical exam for syndromic features
- Bone age X-ray
- Hormonal assessment (TSH, LH/FSH, IGF-1)
- Genetic studies if a syndrome is suspected
Management:
- Treat underlying endocrine cause (e.g., thyrotoxicosis, precocious puberty)
- Monitor and reassure in normal variants
- Genetic counseling and supportive care in syndromic conditions
- Rarely, height reduction therapy is considered (ethical and clinical considerations apply)
Timely evaluation helps differentiate benign tall stature from syndromic or endocrine conditions requiring management.
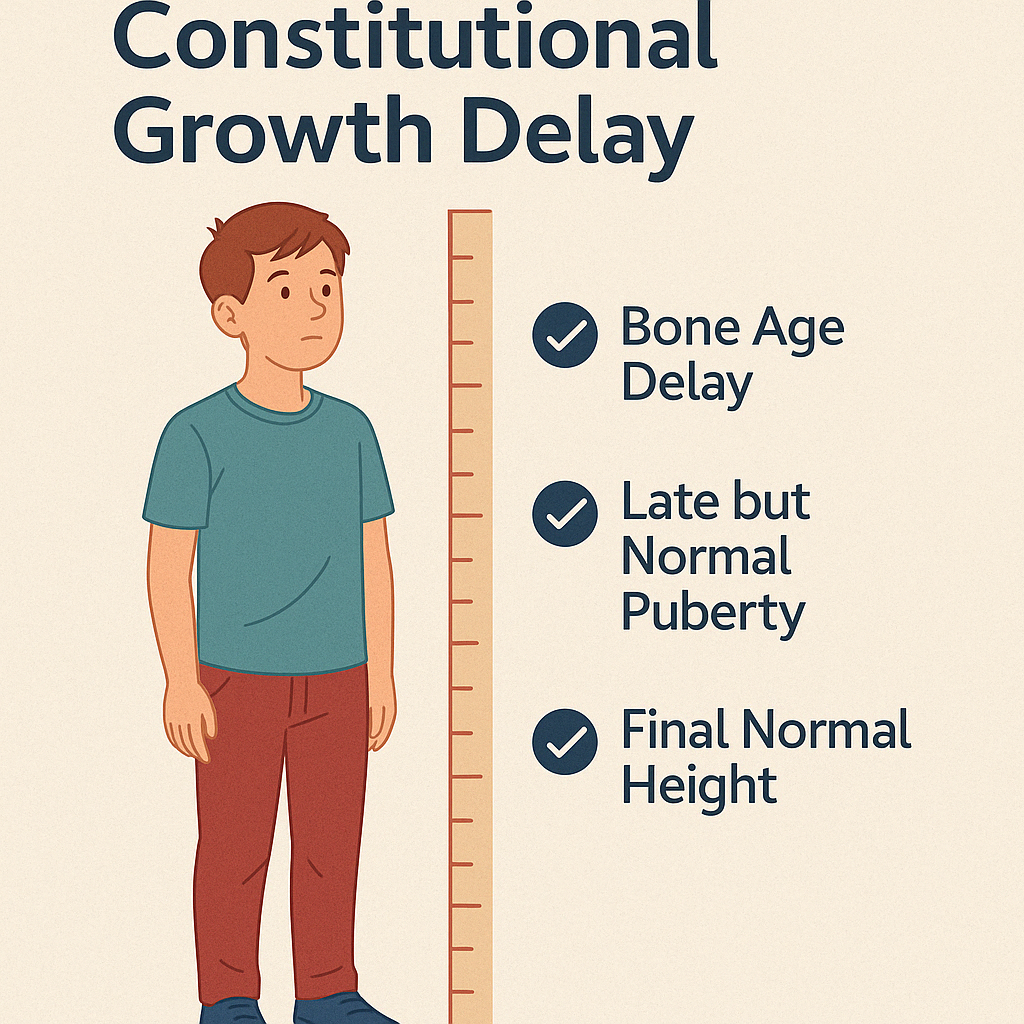
5. Constitutional Growth Delay
Constitutional Growth Delay is a normal variant of growth where a child grows at a slower rate during early childhood but eventually catches up and achieves normal adult height. It is one of the most common causes of short stature and delayed puberty in otherwise healthy children.
Etiology and Pattern
- Often familial — one or both parents may have had delayed growth or puberty
- The child has normal birth weight and height, but growth slows after infancy, resulting in short stature during early years
- Bone age is delayed, typically matching height age rather than chronological age
- Puberty is also delayed but eventually occurs spontaneously and progresses normally
- Final adult height is typically within the normal range
Clinical Features
- Short stature in childhood
- Slower growth velocity
- Late onset of secondary sexual characteristics
- No systemic illness or dysmorphic features
- Normal physical and intellectual development
Diagnosis
- Detailed growth chart analysis
- Bone age X-ray (shows delayed maturation)
- Normal hormone levels (GH, IGF-1, thyroid, cortisol)
- Exclusion of other causes of short stature or delayed puberty
Management
- Reassurance and observation in most cases
- Psychological support if social or emotional distress is present
- Short course of low-dose sex steroids may be used to initiate puberty in selected adolescents
- Rarely, growth hormone is considered if height is extremely low and growth is very delayed
CGD is a benign condition that requires patience, monitoring, and supportive care, not aggressive medical intervention.